MDC Publication Highlights - October 2018
1 November 2018
October 2018 MDC publication highlights: Specific speech-generation deficit in parkinsonism, Genetics of Parkinson's age of onset, Neurological effects of GBA mutations, Cerebellar dysfunction mechanisms in Myoclonus-dystonia & Screening tool for movement disorders in psychosis
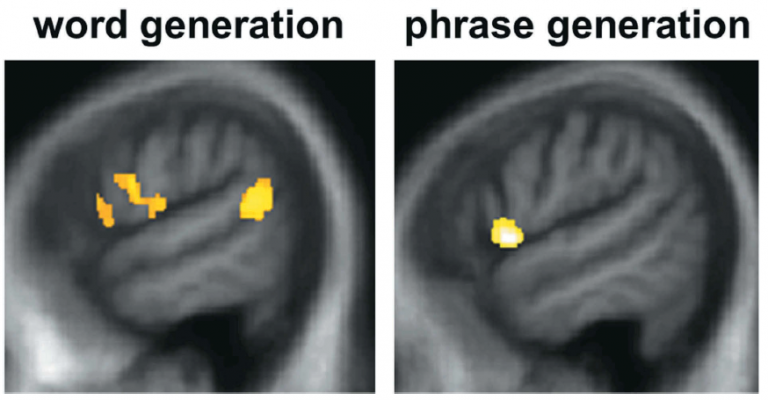
Specific speech generation deficit in parkinsonian syndromes with cognitive impairment
Neurodegenerative parkinsonian syndromes are a group of disorders which, while varying in clinical presentation, all include signs of a Parkinson’s-like pathology combined with cognitive impairment. Problems of speech and language are common in all these conditions but the specific types of linguistic deficits in each condition are not well defined. In this study, the researchers hypothesized that the specific patterns of speech/language impairments in parkinsonian syndromes might be a used for clinical diagnosis and to shed light on disease mechanisms. The researchers focused on patients’ difficulties with generating spontaneous “conversational” speech (verbal adynamia) and sought to investigate how this deficit manifests in different parkinsonian syndromes (vs. “typical” Parkinson’s) and how it interacts with other types of cognitive dysfunction. The study found that patients with parkinsonian syndromes and associated cognitive impairment indeed had impaired speech production, and that this deficit was specific and not related to other language or cognitive deficits. The researchers also found that dopaminergic medication (anti-parkinsonian drugs) significantly improved speech production, while having no direct effect on other cognitive functions, suggesting a relatively specific effect of the drugs on verbal output. These findings highlight a category of language symptoms that is likely to have been under-recognized until now. Impaired ability to generate fluent verbal messages might have potentially profound effects on everyday communication for patients and carers. Conversational speech production should therefore warrant further investigation in order to determine how it contributes to daily life disability, its potential as a disease biomarker and how it may be treated.
Magdalinou et al. ‘Verbal adynamia in parkinsonian syndromes: behavioral correlates and neuroanatomical substrate’. Neurocase, First published: 6 October 2018. doi: 10.1080/13554794.2018.1527368
Genetic factors predicting age of onset in Parkinson’s disease
MDC researchers, working as part of the collaborative International Parkinson’s Disease Genomics Consortium (IPDGC), carried out genetic investigation (genome-wide association studies; GWAS) to find genetic factors that could predict the age of disease onset in Parkinson’s disease. Researchers found that only some genes known to be associated with increased risk of Parkinson’s also had an effect on age of onset, while others did not. Specifically, genes that directly or indirectly influence alpha-synuclein protein aggregation were more likely to affect age of disease onset. These findings support a model in which alpha-synuclein and lysosomal mechanisms impact not only PD risk but also age of disease onset and highlights that therapies that target alpha-synuclein aggregation are more likely to be disease-modifying than therapies targeting other pathways.
Blauwendraat et al. ‘Parkinson disease age of onset GWAS: defining heritability, genetic loci and a-synuclein mechanisms’. BioRxiv, First published: 11 October 2018. https://doi.org/10.1101/424010
Neurological effects of GBA mutations: Gaucher disease and Parkinson’s disease
The association between Gaucher and Parkinson’s disease has been well established for the past 20 years: mutations in the GBA gene, which cause Gaucher disease are also the most common genetic risk factor for Parkinson’s disease (up to 20% of Parkinson’s patients may carry GBA mutations in some ethnic groups). In this review, MDC researcher Prof. Tony Schpaira, world leading expert on GBA mutations and Parkinson’s disease, discusses the clinical, biochemical and genetic basis of GBA-related Parkinson’s disease and Gaucher disease, highlighting commonalities and distinctions between them. The authors consider the evidence for a unifying disease mechanism underlying these conditions, and its implications for future development of disease modifying therapies.
Mullin et al. ‘Neurological effects of GBA mutations’. European Journal of Neurology, First published: 13 October 2018. https://doi.org/10.1111/ene.13837
Mechnisms of Cerebellar dysfunction underlying DYT11 Myoclonus-dystonia
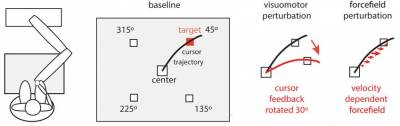
Myoclonus-dystonia syndrome is a rare movement disorder usually caused by mutations in the DYT11 gene. Unlike many other movement disorders, this condition is not associated with neuronal death (neurodegeneration) and is thus thought to be caused by some form of dysfunction in brain circuits responsible for movement. While the nature of the brain dysfunction causing Myoclonus-dystonia syndrome in unknown, a recent and compelling line of research suggests that the cerebellum is primarily involved. Previous studies have shown that patients with Myoclonus-dystonia syndrome have specific difficulties making rapid changes in their eye movement trajectories (e.g., when moving their eyes to find a moving visual target) – a task which is known to be selectively controlled by the cerebellum. In the current study, the researchers wanted to find whether Myoclonus-dystonia patients had a similar difficulty adapting their hand movements when trying to reach a target. Results of the investigation indicated that patients had no impairment in making hand movement adaptations, indicating that the eye movement impairment was highly selective and specific for this group of patients. The authors suggest potential mechanisms at the root of this discordance and discuss the implications of these findings for theories on the role of cerebellar dysfunction in DYT11.
Sadnicka et al. ‘Delineating Cerebellar Mechanisms in DYT11 Myoclonus-dystonia’. Movement Disorders, First published: 17 October 2018. doi: 10.1002/mds.27517
New screening tool for detection of movement disorders in patients treated with antipsychotic medication
Patients with established psychosis treated with antipsychotic medication are at risk of developing a range of movement disorders (including parkinsonism, tardive dyskinesia and others). Some forms of movement disorders may appear shortly after the beginning of antipsychotic exposure, while others may appear after many months or years of drug treatment. Despite their profound effect on patients’ quality of life, movement disorders associated with antipsychotic treatment are still largely underrecognized, mostly due to a lack of a simple and reliable instrument for systematic screening of patients. In this study, a team of neurologists, psychiatrists and mental health nurses, led by MDC researcher Prof. Kailash Bhatia, suggest a new clinical procedure performed by mental health nurses in community services, the ScanMove instrument, for the detection of of movement disorders in patients receiving antipsychotic medication. The new assessment tool is a 31-item screening procedure, whose reliability and validity were measured by ratings of 13 mental health nurses for 635 community patients with diagnostic judgement of a movement disorder neurologist. The ScanMove instrument demonstrated good feasibility and interrater reliability, and acceptable sensitivity as a mental health nurse-administered screening tool for parkinsonism and hyperkinesia in patients with established psychosis.
Balint et al. ‘Development and clinimetric assessment of a nurse-administered screening tool for movement disorders in psychosis’. BJPsych Open, First published: 27 September 2018. https://doi.org/10.1192/bjo.2018.55.
 Close
Close

