Liver transplantation is a surgical procedure where a diseased or damaged liver is removed and replaced with a healthier organ from a donor.

It is usually performed on patients who have a shortened life expectancy due to liver disease. We select recipients who we anticipate will have a good outcome after transplant, compared to their outlook if they do not have a transplant.
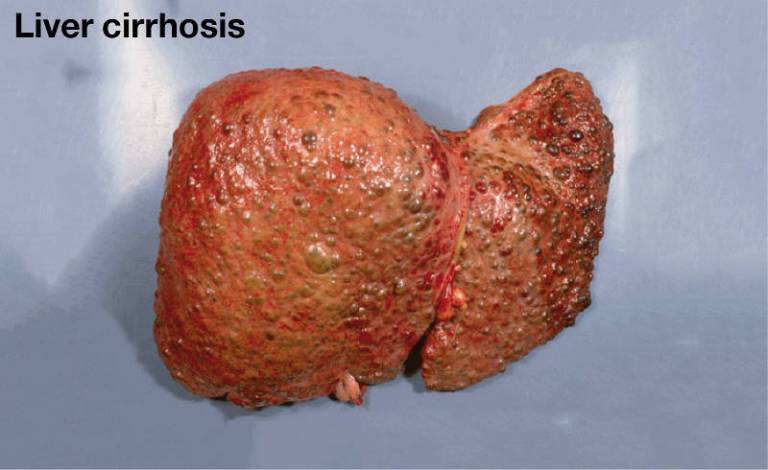
About 90% of liver transplants are done for liver cirrhosis. Liver cirrhosis is scarring of the liver due to continuous, long-term liver damage. Scar tissue replaces healthy tissue and prevents the liver from working properly.
Liver cirrhosis is the end result of many long-term liver dieases. The commonest are fatty liver disease (alcohol and non-alcohol related), infection with chronic viral hepatitis and autoimmune liver diseases.

After a liver transplant, patients require long-term drug treatments called immunosuppression to prevent rejection of the liver. These medicines have potentially negative side effects.
We have to balance the need for drugs against their possible side effects. We are researching ways of tailoring immunosuppression to individual requirements after organ transplantation to reduce the potential harm of these medications.
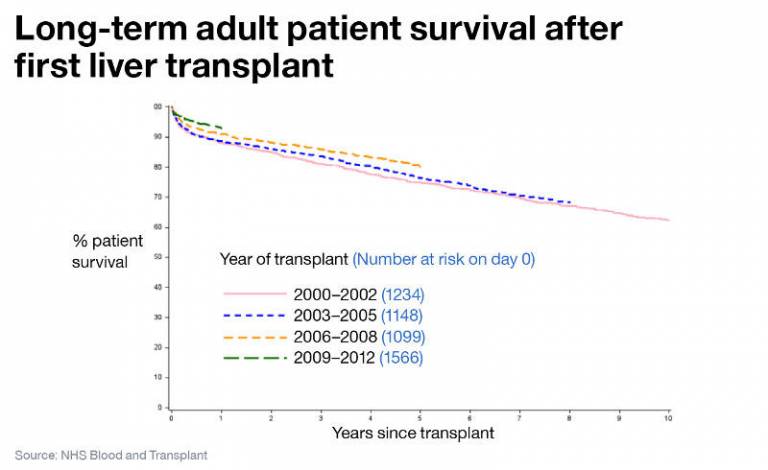
Despite the challenges of liver transplantation we achieve excellent outcomes. 90% of patients are alive after one year and 80% are alive after five years.
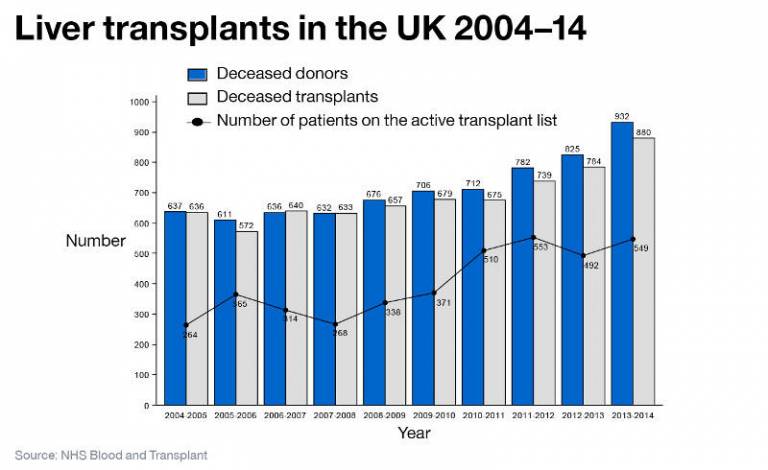
The number of transplants has been rising due to strategies to increase organ donation in the UK, but the number of patients listed for liver transplant far outweighs the number of transplants performed. Around 17% of patients on the liver transplant list die or become too sick to be transplanted.
The following approaches are in place to ensure more UK patients can receive liver transplants: 1) the use of moreo marginal donors from deceased donors; 2) strategies to better preserve organs during transfer from donor to recipient; 3) splitting of donor livers to provide transplants to two recipients; 4) the development of live donor programmes.
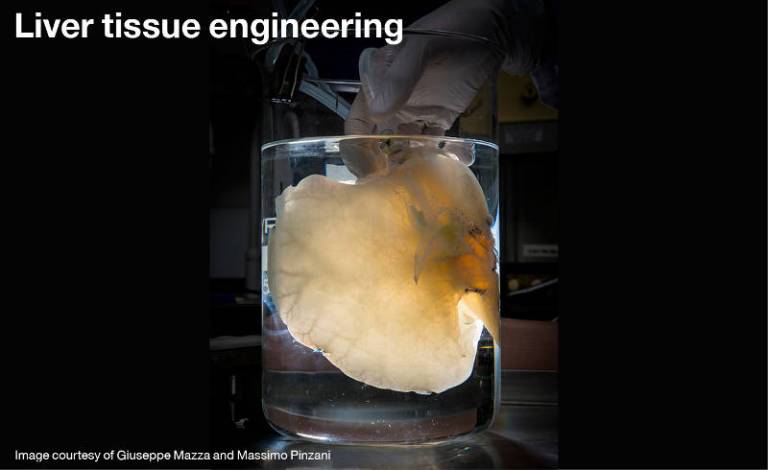
The future of organ tranplantation will likely depend on tissue engineeing. This involves developing human liver scaffolds that do not contain liver cells, and repopulating them with healthy human liver cells. This is a very active area of research within the Institute, alongside the UCL Institute for Liver & Digestive Health.
 Close
Close

