Surgical robots and robotic assisted imaging
11 January 2018
New advancements in robotics technology are transforming the way that surgery is performed.
A surgeon’s tools have come a long way since the crude blades and saws of the 18th and 19th century. Great advancements in technology have meant that is now not uncommon to see robotic systems in operating theatres and clinics assisting with healthcare procedures. This is an area of growth that seems unlikely to slow down; estimates have projected that the market for medical robotic systems will exceed $17 billion by 2020.
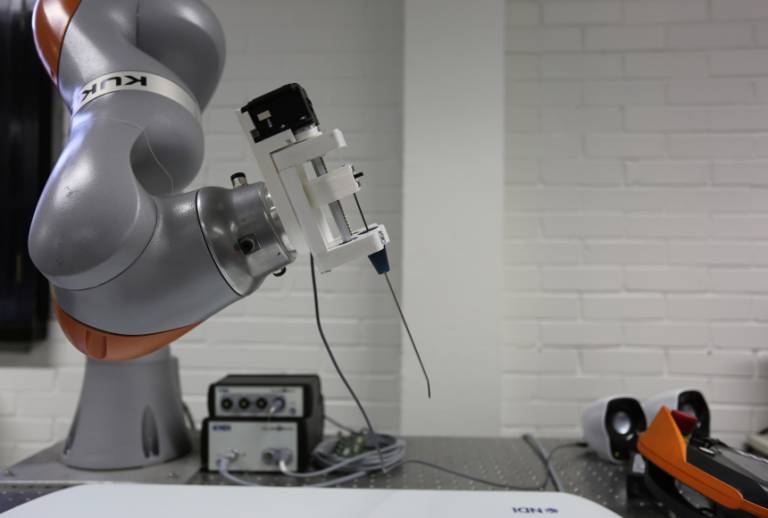
One particularly exciting intersection of research is the marriage of surgical robotic technologies and medical imaging. Whilst robotic systems are frequently used in minimally invasive surgery, imaging inside the body is restricted by the access port. Robotic assisted imaging works to overcome this limitation by combining the autonomy and actuation capabilities of robots with innovative new imaging techniques. This can aid with detection of disease and allow surgeons to navigate and operate with greater precision. We are delighted to be able to showcase an example of this at our exhibition stand at New Scientist Live (28th September – 1st October). Please visit us at stall 1229 to watch our Kuka arm robot with an endoscope in action and hear more about our related research.

GIFT-Surg’s use of robotics in fetal surgery
Teams at UCL are looking at ways in which the Kuka arm and other surgical robots can be incorporated to advance research understandings and capabilities. A research project called Guided Instumentation for Fetal Therapy and Surgery (GIFT-Surg) is working on applying these new technologies to fetal surgery. GIFT-Surg is led by UCL in collaboration with KU Leuven in Belgium, Great Ormond Street Hospital, University College London Hospital NHS Foundation Trust and UZ Leuven.
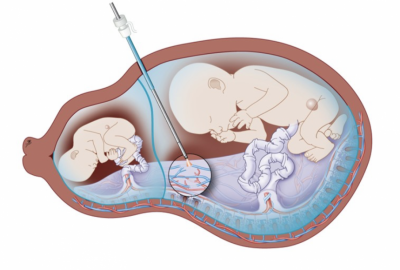
A particular fetal condition that the GIFT-Surg team are using surgical robotics to assist with is twin-to-twin transfusion syndrome (TTTS). TTTS is a complication affecting 10-15% of identical twins who share the same placenta. The disease is caused by the presence of abnormal blood vessels (anastomising vessels) in the shared placenta leading to an imbalance in the blood circulation between the twins. The condition results in uneven transfusion meaning that the donor twin is often underweight and anaemic due to deprivation of blood, whilst the recipient twin’s heart is strained by overload of blood.
TTTS is currently treated in minimally invasive surgery through the insertion of a foetoscope to identify the anastomising vessels, followed by the cauterisation of these vessels with a laser coagulator (see image below). One of the primary challenges of this surgery is the limited field view of the fetoscopic video guidance, worsened by the cloudy amniotic fluid in the womb and instability of imaging caused by movement. The poor visibility hinders surgeons’ ability to accurately locate and cauterise all abnormal vessels. GIFT-Surg researchers are developing technology that combines novel image analysis techniques with advancements in surgical robotics. Using mosaicking it will generate a full 3D model of the placenta from a series of limited 2D fetoscopic images, enabling more accurate navigation and cauterisation.
How can robotic assisted imaging help improve the effectiveness of cancer screening campaigns?
Cancer is the leading cause of death worldwide, accounting for around 13% of total deaths. Screening for cancer is so important because it allows for early detection and treatment of the disease, drastically improving patients’ survival rates. As a result of this there has been a real push in healthcare towards encouraging mass cancer screening campaigns, in both high-income and low-income countries. However, there are many factors that have limited the effectiveness of these campaigns including reluctance of patients and lack of resources. Researchers are increasingly taking an interdisciplinary approach to tackle these challenges, using engineering techniques and innovative robotic technologies to help improve screening processes. To demonstrate this, we are going to look more at two very different projects that Dr Danail Stoyanov, who leads UCL’s Surgical Robot Vision group, is helping collaborate on.

Colorectal diseases like colorectal cancer (CRC) affect a significant number of people worldwide, with an especially high incidence rate in high-income countries. Early diagnosis of CRC is particularly crucial with a 90% survival rate compared to a less than 7% survival rate for those with advanced disease. For this reason, regular screening is recommended to patients who are older or have a family history of CRC. The screening process most commonly used is a colonoscopy, which involves steering a long semi-rigid tube through the patient’s colon. However, the invasiveness, discomfort and frequent pain caused by this procedure leaves many patients reluctant to attend regular screenings, whilst the steering technique itself is difficult to learn and subjectively dependent on the skill of the operator.
The EndoVESPA project (Endoscopic Versatile robotic guidancE, diagnoSis and theraPy of magnetic-driven soft-tethered endoluminAl robots) aims to overcome these challenges by developing an integrated robotic platform for the navigation of a soft-tethered colonoscope that could help diagnosis and treat patients painlessly. The EndoVESPA colonoscopic methodology uses sensing strategies and magnetic control to navigate the endoscope through the colon, eradicating the feeling of discomfort caused by conventional colonoscopy techniques. The hope is that this painless procedure will increase patients’ acceptance of the process, enhancing the effectiveness of mass screening campaigns. EndoVESPA’s research consortium includes Scuola Superiore di studi universitari e di perfezionamento Sant’Anna (SSSA), UCL, EKYMED medical device, Ovesco Endoscopy AG, Universita’ di Torino and University of Edinburgh.
In other areas of the world, effective screening for cancer faces other challenges which robotic assisted imaging could help to solve. For instance, gastric cancer is the second leading cause of cancer death worldwide. Whilst screening programmes have been shown to be incredibly effective in reducing mortality rates through early detection and treatment, they have been particularly hard to carry out in rural and underdeveloped areas. This problem is especially potent in rural China where high levels of gastroesophageal cancer coincide with a shortage of medical resources and personnel over vast distances, leading to higher mortality rates than in any other country.
To tackle this, a multidisciplinary team of researchers led by Prof Pietro Valdastri at the University of Leeds have developed robotic capsule endoscopes which are soft-tethered, swallowable and, crucially, ultra low-cost. The miniature “pill camera” is portable and can be swallowed comfortably without sedation, enabling the screening process to be carried out effectively by volunteers in low-resource areas rather than needing doctors. After each procedure the capsule outer shell and soft tether are discarded, leaving the small endoscopic camera to be reused. The team estimates that this will allow a target cost per procedure of just £2, compared to a capital cost ca. £400 vs £80,000 for existing technology. These features mean that this research has the potential to completely transform the gastric cancer screening process in rural China, enabling far more procedures and saving many lives through early detection. If successful, this platform could be extended much more widely across other low-and-middle-income countries too.
Surgical Robotics at UCL
The cutting-edge research taking place at UCL in surgical robotics and robotic assisted imaging is supported by UCL Robotics and the Surgical Robot Vision research group. As this field grows the boundaries of what is possible in surgical robotics continue to be pushed, enabling these innovative new technologies to deliver patient-focused results.
 Close
Close

