IHI study finds limited association between ACE-inhibitor and ARB medication and incidence of Flu
12 May 2020
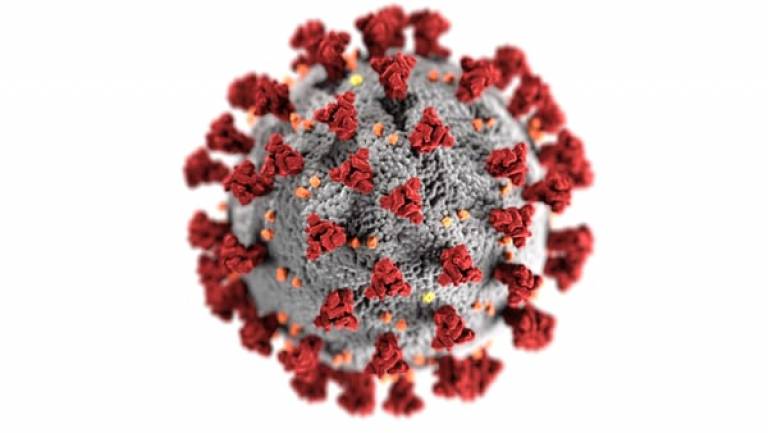
The COVID-19 pandemic has caused significant loss of life and uncertainty worldwide. In the US and the UK, the number of cases continue to rise, and we urgently seek effective medication to treat the disease, especially with older patient with co-morbidities who are at higher risk of poor outcome. In early March, there was speculation on the safety of use during the pandemic for two commonly prescribed medications for hypertension and heart failure, the angiotensin converting–enzyme (ACE) inhibitors and angiotensin-receptor blockers (ARBs). These medications alter expression of ACE2, and coronaviruses engage ACE2 for cell entry and subsequent lung damage. The latter was also observed in influenza A viral infection. IHI researchers Dr Sheng-Chia Chung and Dr Reecha Sofat together with Dr Rui Providencia from Barts Health NHS Trust analysed the anonymous clinical information of 5.6 million people in the UK to investigate the association between use of ACE inhibitor and incidence of influenza. They found that overall ACE inhibitor users had a lower risk of influenza compared to non-users. Since the use of ACE inhibitors was long-term, they performed additional analyses comparing the incidence of influenza with the duration of medication use and observed a curvilinear relationship between the number of prescriptions days and incident influenza. They performed separate analyses for ARBs using the same method and found similar results. The study authors concluded that use of ACE inhibitors and ARBs was associated with either no effect on the incidence of influenza or a lower incidence, depending on the duration of use. While the association between the use of ACE inhibitors/ARBs and risk of contracting COVID-19 remain unclear and future virology studies are needed, these findings may inform the safety of ACEI/ARB use regarding susceptibility to respiratory infection. Study findings were published in a letter on May 8, 2020 in the New England Journal of Medicine
 Close
Close

