Latest News
Researchers and funders unite to launch centre to tackle kidney disease
15 March 2024
The UCL Centre for Kidney & Bladder Health was formally launched on World Kidney Day 2024 with an afternoon featuring the latest research, attended by the leading research institutions, funders and patient representatives.
Kidney disease is the 10th biggest cause of mortality globally and affects around one in 10 people. In the UK, kidney failure alone accounts for around 3% of the NHS’s budget. Historically underfunded, leading charities recently warned that care costs for kidney disease patients could double to £13.9 billion in the next decade.
The new Centre is the first to join up paediatric and adult care, in recognition of the fact that patients are on a journey that doesn’t stop when they hit adulthood. By pooling funding, resources and expertise, the Centre is choosing collaboration over competition in order to reduce overlaps and drive kidney research forward. Its main aim will be to develop prevention strategies, state-of-the-art diagnostics and treatments for those living with kidney and bladder disease.
An audience of 100 researchers, patients and funders attended the launch of the Centre on World Kidney Day to hear about the on-going kidney and bladder research at UCL.
New research featured at the launch included presentations on kidney transplants and the microbiome and a new class of drugs that has reduced chronic kidney disease progression by over a third.
Additionally, the launch of the new Centre coincides with the publication of a new study authored by UCL academics and the UK Kidney Association. The study found that patients with rare kidney diseases are 28 times more likely to experience kidney failure than those with Chronic Kidney Disease (CKD), suggesting that focusing on rare conditions could significantly reduce the burden of kidney disease on both patients and the NHS.
The Centre is uniquely placed to deliver on these ambitious goals by bringing together discovery research and clinical practice from UCL’s Department of Renal Medicine and the UCL Great Ormond Street Institute of Child Health, with close ties to clinical services at the Royal Free and Great Ormond Street Hospitals. Research will take place in genetics, human development, physiology, chronic kidney disease, transplantation, and bladder issues.
Professor David Long (UCL GOS Institute of Child Health), who co-led the development of the Centre, said: “We are incredibly pleased to bring together the scientific expertise of the Institute of Child Health Kidney Development and Disease Group at the UCL Great Ormond Street Institute of Child Health with the world-leading researchers of UCL’s Department of Renal Medicine.
“The UCL Centre for Kidney & Bladder Health’s core mission is to improve the lives of adults and children living with kidney disease, for which there is currently no cure, through clinical translational research.”
Professor Alan Salama (UCLRenal Medicine) said: “Around 1.2 million people in the UK have kidney disease but aren’t aware of it. I am hopeful that our new Centre for Kidney & Bladder Health will pioneer new advancements that will shift the dial in the treatment and diagnosis of kidney and bladder failure.”
Links
- Professor David Long’s academic profile
- Professor Alan Salama’s academic profile
- Kidney Development & Disease Research Group
- Department of Renal Medicine
- New study on rare kidney diseases from UCL and the UK Kidney Association
- World Kidney Day 2024
- UK Kidney Association
****
Vibrant images showcase key moments of discovery in UCL research
29 February 2024
Eye-catching images by researchers at UCL and Great Ormond Street Hospital (GOSH) that highlight “A Moment of Discovery” have been showcased as part of an annual competition.
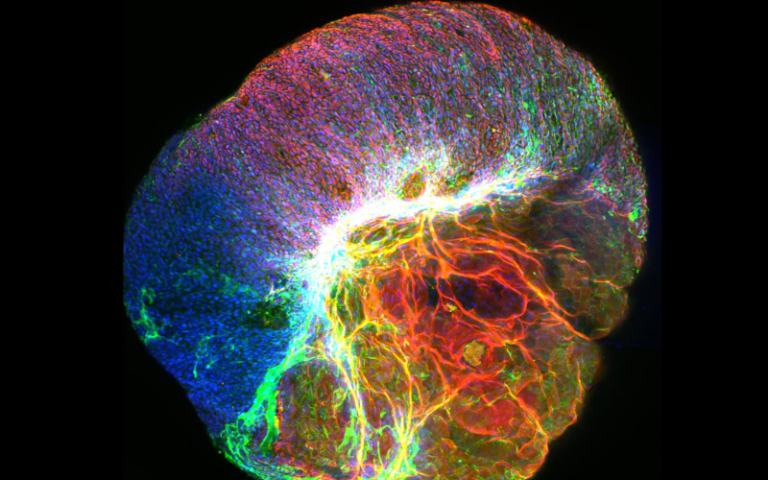
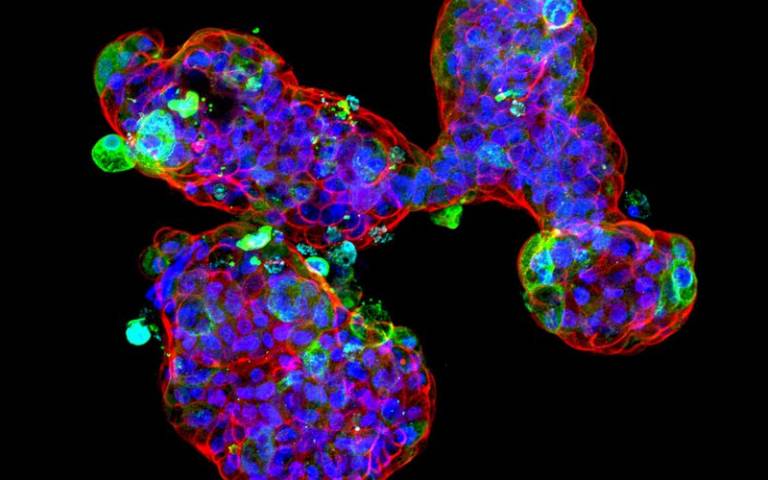
The winning image was submitted by PhD student, Giada Benedetti (UCL Great Ormond Street Institute of Child Health), and shows “The explosive potential of gastrointestinal organoids”.
For the third National Institute for Health and Care Research GOSH Biomedical Research Centre (NIHR GOSH BRC) image competition, staff from the UCL Great Ormond Street Institute of Child Health and GOSH were invited to submit an image of their work that showed “A Moment of Discovery”.
The competition was also open to staff at other children’s hospitals across the UK within the NIHR GOSH BRC paediatric Excellence Initiative.
The eleven images and GIFs offer glimpses into research that is helping to find new treatments for rare or complex conditions and hopes to transform the lives of seriously ill children and young people. They were presented to three panels – the GOSH Young Peoples Advisory Group for Research (YPAG), NIHR GOSH BRC stakeholders and the GOSH staff networks.
The top three images were selected and put to the public who voted for an overall winner via social media.
The winning image shows a gut “mini-organ”, known as an organoid, that is a tiny copy of the digestive system.
During a process used to visualise specific proteins, one of the organoids exploded, revealing its inner workings.
These tiny organs are useful to model gastrointestinal diseases and are the perfect tool for scientists studying new therapies and testing new drugs in the laboratory.
In particular, the organoids can be derived directly from paediatric patients, and this offers the opportunity to test therapies that specifically benefit the child.
Giada Benedetti said: “Sometimes it can be easy to lose sight of why we are performing research, but the close interactions with the hospital really help motivate and give a clear purpose for the work that we do in the lab.
“The image competition is an excellent way to spread awareness for the research and display our scientific findings more dynamically and artistically, which is something that is easily lost in our usual world of number and spreadsheets.”
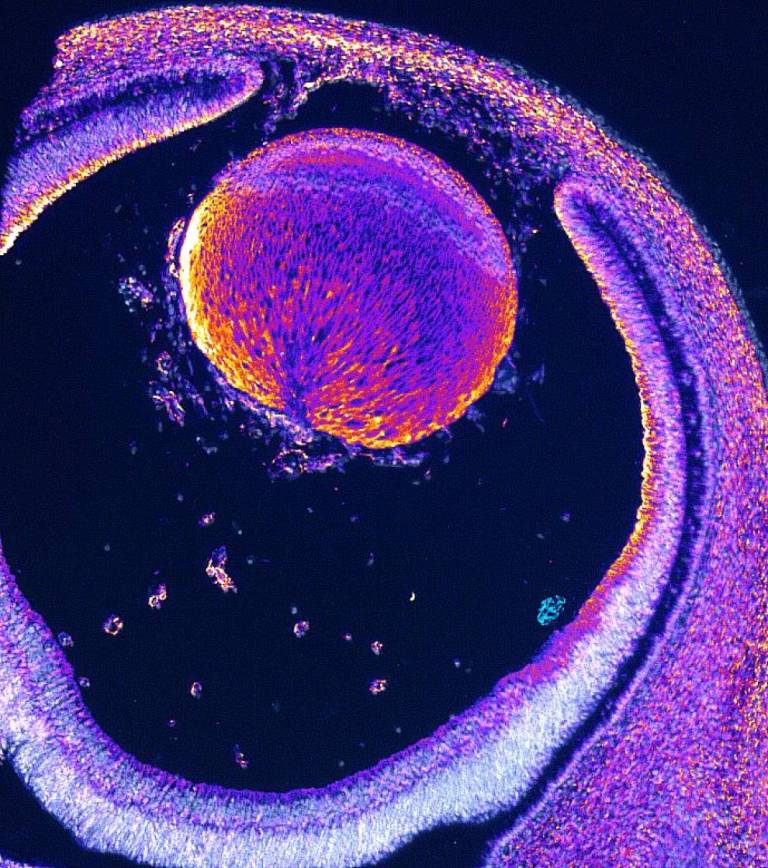
Other notable images included a picture of an embryonic eye stained for dystrophin and an image showing the cells in a knee joint of a child with arthritis.
Links
- UCL Great Ormond Street Institute of Child Health
- UCL Population Health Sciences
- Great Ormond Street Hospital
- NIHR Great Ormond Street Hospital BRC
Images (top-bottom)
- Image ‘The explosive potential of gastrointestinal organoids’ entered by Giada Benedetti, PhD student.
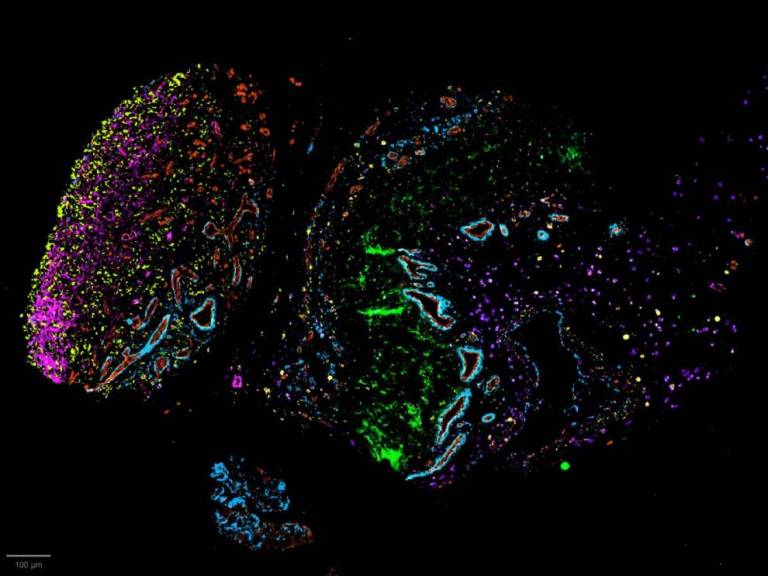
Image ‘what you kneed to know’. Entered by Chrissy Bolton, Soren Lomholt and Patricia Reis-Nis.
Image ‘It’s about seeing the world’. Entered by Reem Alkharji, PhD student.
*****
New target identified for drugs to treat cancer and age-related diseases
29 November 2023
Insights that pave the way for novel therapeutic approaches to tackle cancer, fibrosis, and many age-related conditions have been uncovered by a team of scientists, including researchers from UCL.

The research, published in Nature Cell Biology and led by the Laboratory of Medical Sciences (MRC-LMS), identifies a new target for a class of drugs that selectively eliminate cells that are known to provoke inflammation.
The drugs, known as senolytics, eliminate senescent ’zombie‘ cells that have stopped multiplying in response to either cell damage or ageing. Although senescent cells are inactive, they continue to release proteins that can induce inflammation in the body. Normally the body eliminates senescent cells through the immune system. However, ageing and disease can disrupt this process. Consequently, these cells can accumulate in the body, causing chronic inflammation and tissue disruption.
This further fuels the ageing process and disease development, which in turn generates more senescent cells, forming a vicious cycle.
By removing senescent cells, senolytics reestablish tissue stability, improving the outcome of many age-related diseases.
Though pre-clinical studies have shown some promising results, there are currently no senolytics on the market and those in clinical trials have limitations, creating calls for more effective options to be developed.
Lead author, Professor Jesus Gil (Head of the Senescence Research Group at LMS), said: “In a previous study we showed the potential of repurposing existing drugs, but there are only limited drugs to choose from.
“In this study, we greatly expanded our selection pool by seeking targets in over 7,000 ‘druggable’ genes. We were thrilled to reveal previously unknown vulnerabilities of senescent cells. This opens up new possibilities for treating age-related diseases.”
The team used an approach called RNA interference (RNAi) to assess the molecular pathways influencing the survival of senescent cells. RNAi prevents protein production by reducing gene expression.
They screened RNAi molecules targeting over 7,000 genes and selected the RNAi molecules that selectively killed senescent cells, but not normal cells.
As a result, they identified a senolytic target pathway called coat protein complex I (COPI). Inhibiting this pathway, which is responsible for carrying proteins in the cells, led to the death of senescent cells.
They also showed that targeting this pathway improved outcomes in mouse models of cancer and fibrosis.
Co-author, Professor J.P. Martinez-Barbera (UCL Great Ormond Street Institute of Child Health), said: “When we tested these senolytics in preclinical models of a paediatric brain tumour called craniopharyngioma, we were amazed to see that the majority of the senescent cells had been killed.
“These results have encouraged us to explore these drugs further as potential treatments against these aggressive tumours.”
Building on these findings, the researchers explored drug candidates that target the COPI pathway. Although there are some existing drugs that directly interfere with the COPI pathway, they have limited effectiveness because they only have a short lifespan in the bloodstream, so were not considered suitable for clinical use.
The LMS team collaborated with Professor Edward Tate at Imperial College London and Myricx Bio, an Imperial spin-off, to investigate whether a different class of drugs which indirectly inhibit the COPI pathway, N-myristoyltransferase inhibitors (NMTi), could also target senescent cells. The results were positive- NMTi demonstrated potent senolytic effects, effectively improving the outcome of cancer and fibrosis in mouse models.
Lead author Professor Jesus Gil said: “This work defines a novel class of senolytic drugs that expand the possibilities to treat a wide range of diseases associated with senescence including cancer, idiopathic pulmonary fibrosis (IPF) or non-alcoholic steatohepatitis (NASH).”
The study opens up a new avenue of opportunity to develop drugs which can attack major diseases such as cancer, fibrosis, and other ageing-related conditions. The team is now looking ahead to further research and potential clinical trials, representing a promising advancement in the quest for healthier ageing.
The research was a collaborative effort between LMS, Imperial College London, UCL, The Institute for Research in Biomedicine from Barcelona, University of Southampton and The Francis Crick Institute.
Myricx Bio, an Imperial spin-off, provided access to the NMTi used in the study. UKRI and CRUK were the main funders of this study.
Links
- Research in Nature Cell Biology
- Professor J.P. Martinez-Barbera's academic profile
- UCL Great Ormond Street Institute of Child Health
- UCL Population Health Sciences
Image
- Credit: Murat Photo on iStock
****
Faculty of Population Health Sciences PGR Travel Fund
We are pleased to announce the launch of the Faculty of Population Health Sciences Postgraduate Research Travel Fund.
Applications are now closed.
We will review applications on a rolling basis, in the middle of each month, and aim to provide a decision on funding by the end of that month. The first review will happen on Wednesday, 14 February. The applications will be considered by our Faculty team, with representation from your department. We may contact you for further information about your application, where necessary.
The funding available is as follows:
- Conference within the UK or Europe – maximum award of £200
- International conference (outside Europe and UK) – maximum award of £350
Eligibility criteria:
- You can apply for funds to travel to a research conference, symposium, or other academic meeting. We do not fund attendance at training courses.
- You must be either presenting a poster or giving an oral presentation at the conference, and this must already be confirmed. The application form requires you to upload your acceptance letter.
- You can use the award to pay for registration fees, travel, accommodation, and/or subsistence costs.
- You are not eligible for this funding if you have recourse to other sufficient funding sources (e.g., as part of your studentship)
- You cannot be awarded from this fund more than once in one academic year (August – July).
- Those who have not yet attended a conference may be prioritised.
Award process:
- If you are successful in your application, you will need to pay your costs up front and then claim the award money from the fund.
Please note: the funds we have available for 2023/24 are very limited and may run out quickly, so please apply soon. UCL’s financial year closes at the end of July, after which we are hoping to replenish the funds for 2024/25.
We will review the award process in summer 2024 and will make any necessary amendments.
If you have any questions about the FPHS PGR travel fund, please contact fphs.education@ucl.ac.uk.
*****
Olivia Hodson Cancer Fund: November 2023: Call for Aplications for Funding
Applications closed Wednesday 10th January 2024
http://www.ohcf.org/
The Olivia Hodson Cancer Fund is a special Purpose Fund within Great Ormond Street Hospital Children’s Charity. The fund was established in 1997 in memory of Olivia Hodson who died from a malignant germ cell tumour in April 1996, aged two and a half years old and is supported by Olivia’s family and their friends. The fund supports projects that would help other sick children and their families in the future and supports cancer related projects within GOSH and ICH.
The OHCF invites applications for funding of projects starting after April 2024. The Fund aims to achieve a balance between larger grants (between £10,000.00 and £20,000.00) and smaller grants (£1000+). The Fund will look favourably on smaller grants that can show measurable impact and we also encourage pump-priming applications for smaller amounts of approximately £1,000.00 to 1,500.00.
Only one application per team or research group will be allowed per call.
Please download document with further information about the fund and the application form. Applications should be emailed to Anne Anton at ich.dbc.admin@ucl.ac.uk by Wednesday 10th January 2024. Applications should be fully costed and registered with R&D.
Your recommended peer reviewers will be contacted shortly after the deadline. It may speed up your application to let them know in advance that we will be getting in touch. The committee are unable to approve applications without a peer review.
The Committee will meet to review applications shortly after the deadline of 10th January when they will shortlist applications to be sent for external review. The committee will meet to assess the applications and reviews in March 2024.
*****
Child Health Research PhD Studentships 2024/25
Developmental Biology and Cancer Projects
- Sex differences in disorders of the embryonic brain
- Design of nanoparticle-based, Toxin Gene Systems For Neuroblastoma Treatment
- The HMMR protein as a potential oncogenic driver in neuroblastoma
- Advancing translational cell therapy for Hirschsprung disease
- Understanding the functional development and plasticity of Interstitial cells of Cajal: Potential targets for gut motility disorders
- Developing artificial mini-kidneys to treat childhood kidney disorders
- Development of new models of Diffuse Midline Glioma in zebrafish
- Skull base malformations in craniofacial disorders
- DNA damage and cell senescence as causes of embryo malformations
- How do neural progenitor cells integrate into the neuroepithelium?
- Developing AAV gene therapy for Polycystic Kidney Disease
- Treating congenital diseases before birth
- Analysing Heart Development Using Stem Cell and Mouse Synthetic Embryoids.
- Unraveling the epigenetic vulnerabilities of recurrent paediatric brain tumours
- Investigating the role of mechanical compression in alveolar specification during fetal lung development.
- Investigating MYB regulated transcriptional circuits to uncover novel leukaemia susceptibilities
- Single cell mapping of the human amniotic fluid across healthy and diseased gestation
******
- Research in EMBO
- Professor Jane Sowden’s academic profile
- Dr James Wawrzynski’s academic profile
- UCL Great Ormond Street Institute of Child Health
- UCL Population Health Sciences
- NIHR Great Ormond Street Hospital Biomedical Research Centre
- Dr Daniyal Jafree's academic profile
- Reem Al-Saadi's academic profile
- Dr Dale Moulding's academic profile
- Dr Tanzina Choudhury's academic profile
- Naima Smeulders's academic profile
- Professor David Long's academic profile
- Professor Kathy Pritchard-Jones's academic profile
- Professor Thomas Voit's academic profile
- UCL Great Ormond Street Institute of Child Health
- UCL Population Health Sciences
- GOSH NIHR GOSH BRC
- Research paper Short-wave infrared imaging enables high-contract fluorescence-guided surgery in neuroblastoma in Cancer Research
- Dr Stefano Giuliani's academic profile
- Dr Dale Waterhouse's academic profile
- Dr Laura Privitera's academic profile
- UCL Great Ormond Street Institute of Child Health
- UCL Medical Physics & Biomedical Engineering
- Professor Marc Mansour's academic profile
- Dr David O'Connor's academic profile
- UCL Great Ormond Street Insitute of Child Health
- Developmental Biology and Cancer Research and Teaching Department
- Faculty of Population Health Sciences
- UCL Cancer Institute
- Faculty of Medical Sciences
- Great Ormond Street Hospital for Children
- Research in Nature Communications
- Dr Giovanni Giobbe's academic profile
- Professor Paolo De Coppi's academic profile
- UCL Great Ormond Street Institute of Child Health
- UCL Population Health Sciences
- NIHR GOSH BRC
- Professor Darren hargrave's academic profile
- Professor JP Martinez-Barbera's academic profile
- Professor Tom Jacques's academic profile
- UCL Great Ormond Street Institute of Child Health
- UCL Population Health Sciences
- Research in Nature Medicine
- Dr Sara Ghorashian’s academic profile
- UCL Great Ormond Street Institute of Child Health
- UCL Population Health Sciences
- GOSH Wellcome Sanger Institute
- Previous news items 2023
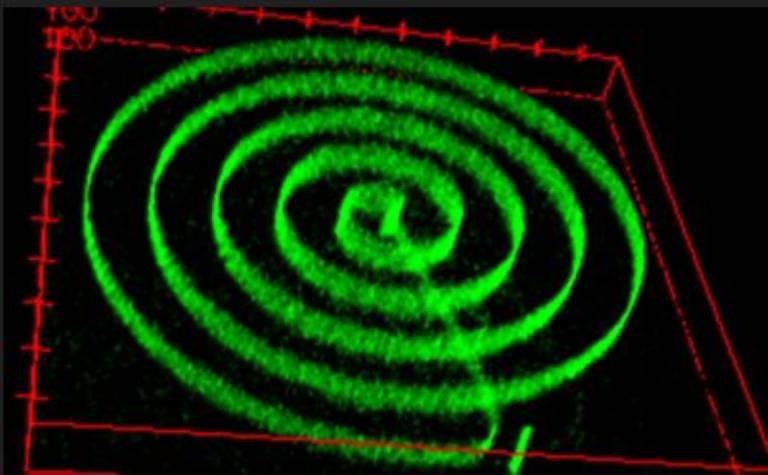
New gene therapy could reduce hearing loss in Norrie disease
6 September 2023
A gene therapy developed in mice by an international team of researchers led by UCL and the NIHR Great Ormond Street Hospital Biomedical Research Centre, could significantly reduce hearing loss associated with Norrie disease.

Norrie disease is a rare but devastating genetic disorder that causes blindness and hearing loss. The condition primarily affects boys.
Children affected by the condition are born blind and develop progressive hearing loss from around the age of 12 years old. The research, published in EMBO, aimed to investigate whether it was possible to slow or prevent this from happening.
Currently, the only possible treatment option to help hearing loss in Norrie disease, is cochlear implants. However, these are only partly effective.
The new research has found that gene therapy can be used to prevent the death of vitally important hair cells in the cochlea (the part of the inner ear responsible for sensing sound) and stop the loss of hearing associated with Norrie disease.
Professor Jane Sowden (UCL Great Ormond Street Institute of Child Health and co-theme lead of tissue engineering and regenerative medicine at the NIHR GOSH BRC), who led the research, said: “I hope that gene therapy for hearing loss caused by faulty genes will soon be available for patients.
“In this study we were able to reduce the progressive hearing loss in a Norrie disease model by gene therapy for the first time. The treatment in mice was successful not only for newborns but also when we treated at a stage comparable to children and young people.
“This is exciting progress as it lays the groundwork for future application in patients – this could be transformative for them and their families and carers.”
To achieve this, the team injected a gene therapy designed to restore the missing norrin protein. They showed that the abnormal blood vessels in the ears and eyes that develop in mice with Norrie disease are improved by the treatment.
Researchers hope that this could help prevent deafblindness as tests showed both better hearing and vision after gene therapy treatment in mice.
Co-author, Dr James Wawrzynski (UCL Great Ormond Street Institute of Child Health), said: “Children with Norrie disease progressively lose their hearing because of a faulty gene called NDP, which is responsible for some of the structures in the inner ear.
“In our study we have shown that in mice with Norrie disease, we can correct this faulty gene by inserting billions of new ‘fixed’ copies into the bloodstream. This gene therapy appears to lead to better blood vessel structure in the inner ear and crucially we can see the sensory hairs are protected.
“Being able to offer effective treatment could be life-changing for children who are seen at hospitals around the world, including at GOSH. Being blind can be challenging but treating or slowing the progression of hearing loss could mean the difference between independence as an adult, or not.”
First author, Dr Valda Pauzuolyte (UCL Great Ormond Street Institute of Child Health), said: “We have previously shown that Norrie hearing loss of the sensory hair cells in the inner ear. While there may also be other factors involved, once lost, cochlear hair cells cannot regrow. This new work shows that NDP gene therapy can be very effective in preventing further damage to the hair cells and hearing in Norrie disease in mice.
“Hearing is one of the most important senses. While sight loss is already established at birth for those with Norrie disease, this work shows how we might be able to help them keep their hearing – an incredibly important sense.”
When this research was initially funded, patient advocacy group the Norrie Disease Foundation, who provide vital support to families living with the condition, commented: "Our hope is that this research will provide a treatment so our blind community don’t also become deaf.
“Currently, families are expected to deal and cope with the symptoms. Now there is a chance that one of the life-changing symptoms can be delayed or even stopped. There is potential for a brighter future for Norrie patients, and this gives a feeling of optimism. Whilst Norrie disease can’t currently be cured, it feels like we are one step closer to making the condition less devastating."
This research was funded by GOSH Charity, the NIHR GOSH BRC, which underpins all research at GOSH, Newlife the Charity for Disabled Children, SPARKS, and the Royal National Institute for Deaf People.
Links
Research in EMBO Professor Jane Sowden’s academic profile Dr James Wawrzynski’s academic profile UCL Great Ormond Street Institute of Child Health UCL Population Health Sciences NIHR Great Ormond Street Hospital Biomedical Research Centre****
Images
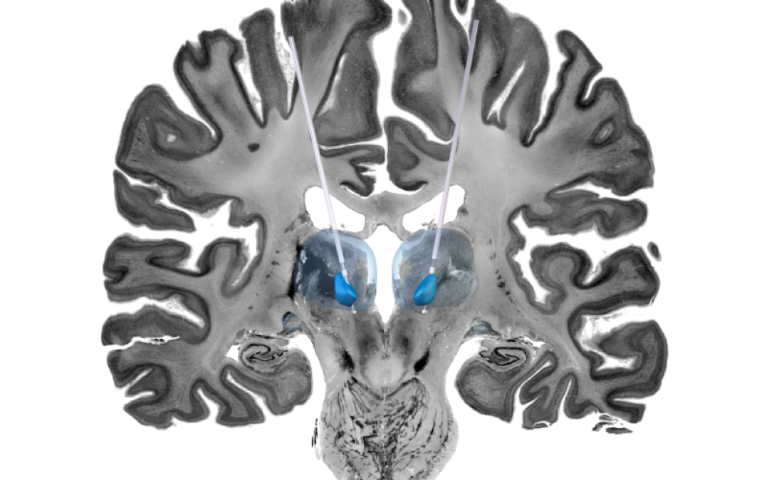
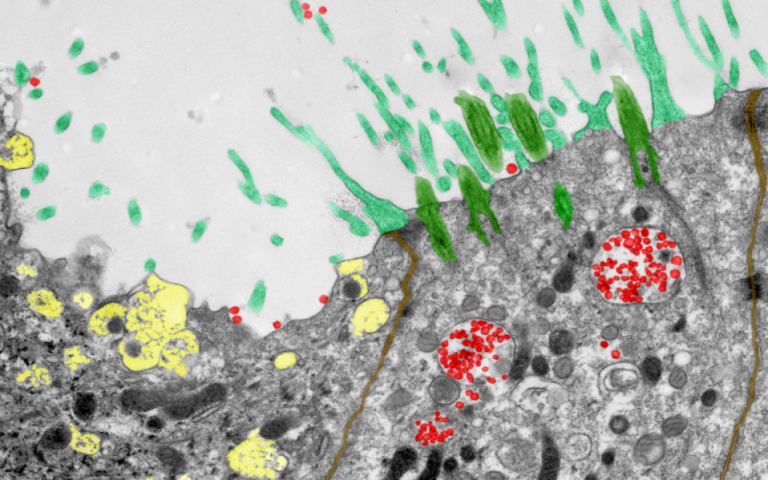
A 3D snapshot of the hidden highways in childhood kidney cancer by Dr Daniyal Jafree, Aleksandra Letunovska, Reem Al-Saadi, Dr Dale Moulding (UCL Great Ormond Street Institute of Child Health), Radu Polschi (UCL Medical School), Dr Tanzina Choudhury, Dr Ciaran Hutchinson and Miss Naima Smeulders (GOSH). Stimulating the brain, an evolving treatment for children with drug-resistant seizures by Professor Lewis Spitz and PhD candidate Rory Piper (UCL Great Ormond Street Insitute of Child Health). CADET Project Nasal COVID-19 factories by Dr Maximillian Woodall and Dr Samuel Ellis alongside Dr Andrea Pinto from Leica Microsystems.****
Images showcase life-changing UCL research
2 March 2023
Images that highlight UCL research have been showcased in an image competition run by Great Ormond Street Hospital for Children (GOSH).
Researchers from UCL Great Ormond Street Institute of Child Health, UCL Medical School and GOSH were named the winners of the annual research and innovation image competition - named ‘A Moment of Discovery’.
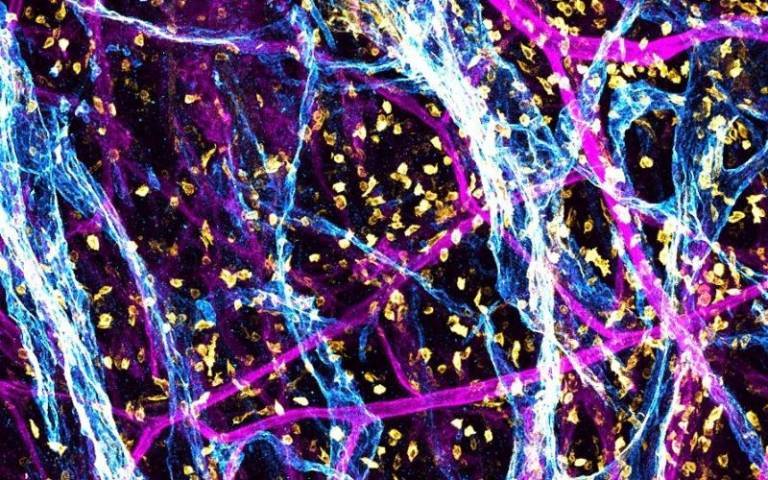
The winning image, titled ‘A 3D snapshot of the hidden highways in childhood kidney cancer’, is a 3D microscope image of a stained kidney tumour removed after surgery at GOSH. The image show the tumour lymphatic network (coloured blue) that is responsible for draining waste and cells, amongst blood vessels (in magenta) and immune cells (in yellow).
The team who submitted the image includes Dr Daniyal Jafree, Aleksandra Letunovska, Reem Al-Saadi, Dr Dale Moulding (UCL Great Ormond Street Institute of Child Health), Radu Polschi (UCL Medical School), Dr Tanzina Choudhury, Dr Ciaran Hutchinson and Miss Naima Smeulders (GOSH).
The research, which is led by Professor David Long and Professor Kathy Pritchard-Jones (both UCL Great Ormond Street Institute of Child Health), focuses on how cancers grow and spread through these vessel networks, with the hope of understanding whether the size of the network can predict how well children respond to chemotherapy, or if these highways influence the likelihood of the cancer spreading.
Structures like lymphatic vessels are incredibly hard to see in their entirety using traditional microscope techniques. However, through collaboration, the team brought their unique skills together to generate this image using a new 3D imaging technique to view the complete lymphatic vessel network within the tumour in high detail, to better understand how cancers can grow and spread.
Dr Daniyal Jafree said: “I’ve been working at UCL Great Ormond Street Institute for Child Health for seven years, and in that time, two things have become very clear. Firstly, it’s so important that we communicate our research to the people we ultimately hope to benefit: patients, their families and the public.
“Secondly, none of our research would be possible without a big team of scientists and clinical professionals, all with different backgrounds and experiences, all sharing the common goal of improving diagnosis and treatment for childhood diseases and cancer.
“The team and I are really pleased that our image, which showcases just how important these two things are to research and innovation, was voted as favourite by the public.”
The competition, run by GOSH and the National Institute for Health and Care Research GOSH Biomedical Research Centre (NIHR GOSH BRC) shortlisted 11 images that offer glimpses into the huge array of research underway at the hospital and its partners to develop better treatments for seriously ill children.
Other images in the top three were also submitted by academics from UCL GOS ICH, including an image showing the cross-section of a stimulated brain used to help study potential treatments for epilepsy in children by Professor Lewis Spitz and PhD candidate Rory Piper, and human nose cells infected with SARS-CoV-2 by Dr Maximillian Woodall and Dr Samuel Ellis alongside Dr Andrea Pinto from Leica Microsystems.
Hundreds of people voted for the winning image on social media.
In celebration of Rare Disease Day, all shortlisted images are being exhibited in the entrance of the Zayed Centre for Research into Rare Disease in Children (ZCR). These are available to view from the street, along with a one-of-a-kind laboratory in a dropped floor that is home to the researchers that work on some of the most rare and complex conditions in children.
The competition was open to staff from across GOSH and its affiliated institutes including the NIHR GOSH BRC and UCL GOS ICH. This year the competition was also opened to children’s hospitals across the UK within the NIHR GOSH BRC Paediatric Excellence Initiative, including Alder Hey, Birmingham and Sheffield.
Professor Thomas Voit, Director of NIHR GOSH UCL Biomedical Research Centre, who was on the panel, said: “These images are stunningly beautiful and vivid reminders of how intricately organised the microcosm of biology is.”
Links
Dr Daniyal Jafree's academic profile Reem Al-Saadi's academic profile Dr Dale Moulding's academic profile Dr Tanzina Choudhury's academic profile Naima Smeulders's academic profile Professor David Long's academic profile Professor Kathy Pritchard-Jones's academic profile Professor Thomas Voit's academic profile UCL Great Ormond Street Institute of Child Health UCL Population Health Sciences GOSH NIHR GOSH BRCImage
iStock. Credit: stefanamer****
Lighting up tumours could help surgeons remove them more precisely
20 March 2023
A new technique that combines highly detailed, real-time images of inside the body with a type of infrared light has, for the first time, been used during surgery to differentiate between cancerous tumours and healthy tissue.
The pioneering technique, demonstrated in mice, has been developed by engineers at the Wellcome/EPSRC Centre for Interventional and Surgical Sciences (WEISS) at UCL and surgeons at Great Ormond Street Hospital (GOSH).
Researchers say the development could have implications for treating neuroblastoma, which is the most common form of solid cancer tumour, other than brain tumours, found in children. Standard treatment typically involves surgery to completely remove cancerous cells, which can be difficult to see as they look similar to the surrounding healthy tissue.
For the study, published in Cancer Research, scientists at UCL and GOSH used a technique called ‘molecular imaging’ during surgery, where chemicals are injected into the bloodstream to act as imaging probes. These chemicals are attracted to cancerous cells in the body, and once attached, the probes light up through a process called ‘fluorescence’, which in turn lights up the tumour. The technique, used during preclinical testing in mice, successfully revealed part of a tumour that had not been removed during surgery.
Next the team wanted to test whether they could improve the visual quality of the images, by using a ‘new’ type of light, short wave infrared light (SWIR), that has only recently become accessible to scientists through new technology.
For this they used a special high definition camera to capture SWIR fluorescence. SWIR is invisible to the naked eye and has a longer wavelength than visible light, allowing it to penetrate deeper into the tissue to provide sharper, more detailed images. Using this technique, surgeons were able to distinguish between cancerous tumours and healthy tissue during the preclinical tests.
Team leader Dr Stefano Giuliani, Consultant Paediatric Surgeon at Great Ormond Street Hospital and Associate Professor at UCL Great Ormond Street Institute of Child Health, said: “Surgery to remove neuroblastoma requires a delicate balance. Remove too little and the tumour might grow back, but remove too much and the surgeon risks damaging the surrounding blood vessels, nerves and other healthy organs. This technique effectively lights up the tumour, allowing surgeons to remove it with unprecedented precision. We hope to be able to translate this innovative technology into clinical practice at GOSH as soon as possible to benefit the largest number of children with cancerous tumours.”
Neuroblastoma is a devasting childhood cancer and accounts for 8-10% of all childhood cancers and around 15% of childhood deaths from cancer. In around a third of patients the cancer has already spread to other parts of the body at the time of diagnosis, making it harder to treat.
Unlike X-ray or magnetic resonance imaging (MRI), which focus on organs and bones, molecular imaging produces detailed pictures of biological processes, and can be done live during surgery, meaning clinical teams don’t have to wait for biopsy or culture results when screening for diseases. The SWIR enhances the images in real time.
Dr Dale Waterhouse (Wellcome / EPSRC Centre for Interventional & Surgical Sciences (WEISS) at UCL) said: “This work shows that SWIR imaging, a technology first used for material inspection, can enhance the surgeon’s vision beyond the capabilities of the human eye, allowing more precise tumour surgery. It is very exciting to be part of an interdisciplinary team where surgeons and engineers work together, pioneering cutting-edge technologies that promise to improve the treatment of patients at GOSH.”
Dr Laura Privitera (UCL Great Ormond Street Institute of Child Health) said: “Paediatric surgical oncology faces an ever-increasing need for novel technologies and devices that can help visualise tumours intraoperatively. By using targeted fluorescence-guided surgery, we demonstrate the possibility of safely and specifically delineating tumour margins, allowing its differentiation from surrounding healthy tissue. Fluorescence-guided surgery is a game-changing innovation that will help surgeons to obtain safer and more complete resection. It is exciting to be part of this project, and I look forward to seeing this technology translated into the clinical environment.”
Scientists at GOSH and UCL WEISS are now working to fast-track the technology into the operating theatre at GOSH within the next 12 months to benefit children with cancerous tumours.
The study was supported by the Medical Research Council, WEISS, EPSRC, the Royal Academy of Engineering and GOSH.
Links
Research paper Short-wave infrared imaging enables high-contract fluorescence-guided surgery in neuroblastoma in Cancer Research Dr Stefano Giuliani's academic profile Dr Dale Waterhouse's academic profile Dr Laura Privitera's academic profile UCL Great Ormond Street Institute of Child Health UCL Medical Physics & Biomedical EngineeringImage
Saline intravenous (iv) drip in a child's patient hand. Credit: kdshutterman on iStock
Media contact
Poppy Danby
E: p.danby [at] ucl.ac.uk
*****
Genetic clues could predict leukaemia patients’ risk of treatment failure
5 May 2023
New research led by UCL and Great Ormond Street Hospital (GOSH) to predict which childhood leukaemia patients are at higher risk of not responding well to chemotherapy will allow clinicians to refine treatment strategies to give the best chance of success.
The study, published in the Journal of Clinical Oncology, combined UK trial data from 2003-2019 to see which patients had worse outcomes. They then used whole genome sequencing to look for genetic clues that could be used to predict this risk in future patients.
The team hope that these genetic clues can be used to identify high-risk patients early, who may be eligible to take part in trials for the latest immunotherapies, such as CAR-T cell therapy.
Acute lymphoblastic leukaemia (ALL) is the main type of childhood leukaemia and is split into two subtypes, B-Cell ALL (B-ALL) and T-Cell ALL (T-ALL). The current conventional therapies for ALL include induction chemotherapy and bone marrow transplant. But patients are three times more likely to not respond well to therapy and suffer poor outcomes in T-ALL compared with B-ALL, and there are fewer treatment options available when patients relapse.
This may be about to change, with trials underway for highly promising immunotherapies such as CAR-T cell therapy. This technique was recently used by scientists at UCL and GOSH to treat a patient’s ‘incurable’ T-ALL leukaemia after conventional treatments had failed. Though the trial continues, the patient is still cancer free almost a year after starting treatment.
In the new study, the team analysed data from two clinical trials that involved ALL patients treated in the UK between 2003 and 2019, to see what happened to the patients and identify the risk factors associated with conventional treatment failure.
Frozen cells from these trial patients were then whole genome sequenced in order to look for genetic markers associated with poor outcomes, and which might be used to predict the risk of conventional treatment failure in future patients.
The researchers found that one in five older patients, in this case teenagers and young adults, experienced poor outcomes compared to just one in ten younger patients.
Though the genetic profile of the cancers they studied was complex, with individual cancers often very different from one another, the researchers found that mutations in the TAL1, MYC and RAS molecular pathways could be used to quantify a patient’s risk of treatment failure.
Dr David O’Connor (UCL Cancer Institute and Great Ormond Street Hospital) said: “Genetic stratification, where you analyse a patient’s genome to assess their risk of certain outcomes, has been successfully used to improve B-ALL treatment. But until now we haven’t had the data to do this for T-ALL. Our results could identify a group of high-risk patients who are less likely to respond well to chemotherapy. All childhood leukaemia patients in the UK undergo whole genome sequencing when they are diagnosed, so the genetic information should already be available to do this.”
Genetic stratification of patients to identify those who are less likely to respond well to conventional treatments would mean that they could be considered for alternatives, such as the CAR-T cell therapies that are now available in clinical trials.
Professor Marc Mansour (UCL Great Ormond Street Institute of Child Health and UCL Cancer Institute) said: “Around 10% of paediatric T-ALL patients do not respond to initial chemotherapy and the chance of relapse is twice as high as in B-ALL. This is compounded by the fact that there are fewer treatment options for relapsed T-ALL patients. So in T-ALL it’s even more important to provide the treatment that will give the highest chances of remission. The genetic markers that we’ve identified in this study will allow us to provide the best treatment strategy.”
This research was funded by Blood Cancer UK, Cancer Research UK, GOSH Children’s Charity and Wellcome.
Links
Professor Marc Mansour's academic profile Dr David O'Connor's academic profile UCL Great Ormond Street Insitute of Child Health Developmental Biology and Cancer Research and Teaching Department Faculty of Population Health Sciences UCL Cancer Institute Faculty of Medical Sciences Great Ormond Street Hospital for ChildrenImage
Credit: Urciuolo and Giobbe et alMedia contact
Poppy Danby
E: p.danby [at] ucl.ac.uk
****
3D ‘bio-printing’ inside hydrogels could help understanding of how cancer spreads
9 June 2023
Scientists from across UCL, Great Ormond Street Hospital and the University of Padova have shown how 3D printing can be achieved inside ‘mini-organs’ growing in hydrogels, which could help better understand how cancer spreads through different tissues.
The new technique can help control the shape and activity of the mini-organs, and even force tissue to grow into ‘moulds’. The researchers hope that this will allow teams to produce realistic models of organs and disease, and study cells and organs more accurately.
Organoid science is a particularly promising area of research at the Zayed Centre for Research (a partnership between the UCL Great Ormond Street Institute for Child Health and Great Ormond Street Hospital). It involves the creation of micro-versions of organs such as the stomach, intestines and lungs.
However, the tissue almost always grows in an uncontrolled way and doesn’t represent the complex structure of naturally occurring organs. This is particularly important as an organ’s shape and structure is as crucial as its cellular makeup.
The new research, published in Nature Communications, shows for the first time how scientists can create solid structures within a pre-existing gel to solidify specific patterns in real time, guiding organoids growing in the gel into a particular structure by using light from a high-specification microscope. This means that any cell in the growing mini-organ or entire organoids will grow in a specific and precise way.
For example, to study how cancer travels through tissue of different hardness and density, the team created hardened gel cages around cancer cells and monitored how their movement changed depending on the density of its surroundings – this is important for understanding the spread of cancer.
By creating better models of disease, future studies will be more reliable and have better quality results. Researchers hope this will eventually lead to a reduction in animal research.
The team now plan to use the technique to recreate and study what happens to an organ’s function when it doesn’t grow correctly – for example in many malformations that develop in the early stages of pregnancy.
The work could also lead to treatment through the delivery of biologically accurate ‘patches’ in living organs.
Co-lead author of the research, Dr Giovanni Giobbe (UCL Great Ormond Street of Child Health), said: “It’s been amazing to see these precise structures begin to form before our eyes due to our small but painstaking adjustments in the polymer gel.
“We’re really excited to see where this can take us in the understanding of human disease and one day, treatment.”
To explore the ‘printing’ uses of the technique the team applied the method to several different situations.
For example, to study neurons, organoid research would traditionally create disordered bundles of neurons that are impossible to isolate and study. However, this technique allows the team to create hardened gel ‘rails’ for the neurons to grow along, like the lanes of an Olympic pool.
Meanwhile, to ensure that microscopic intestines are created with the same shape as ‘real’ developing intestines, the team created a complex hydrogel mould that guided organoids into shapes that mimic the complex structure of a developing intestine called ‘crypts’ and ‘villi’.
Similarly, scientists were able to pattern a hydrogel to encourage lung cells to create branches, like they do in a real lung.
Professor Paolo De Coppi (UCL Great Ormond Street Institute of Child Health, paediatric surgeon at GOSH, and co-lead of the tissue and engineering and regenerative medicine theme at the NIHR GOSH BRC), said: “This work is an excellent example of how we can bring interdisciplinary, international teams together to improve our research and benefit patients.
“Teams at GOSH and UCL that specialise in organoid research in the UK, working with Italian teams specialising in design and application of gel-printing, are what have made this incredible and beautiful piece of research come to fruition. This will have implications for laboratory-based research to improve our understanding of disease but could also lead to in-patient uses and treatments.”
Next steps for this work will be to study these controlled, moulded and directed mini-organs to better understand how they can mimic real organs and conditions in the body.
Dr Anna Uriuolo (University of Padova and lead of the Neuromuscular Engineering Lab at the Institute of Paediatric Research) said: “This work in an exemplar of the advancements of the multidisciplinary approach that is exploding in biomedical research. The ability to reproduce models of organs in the lab and the development of technologies that help scientists to recapitulate healthy and diseased tissues and organ complexity on the bench is the outset of how translational medicine will change in the next future.”
This work was funded by 2017 STARS-WiC grant of University of Padova, Progetti di Eccellenza CaRiPaRo, TWINNING of University of Padova, Oak Foundation Award, AFM Telethon, ‘Consorzio per la Ricerca Sanitaria’ (CORIS) of the Veneto Region, Italy (LifeLab Program), European Research Council (ERC, RerOids) to N.E., and the STARS Starting Grant 2017 of University of Padova and IRP Consolidator Grant to A.U., NIHR GOSH Biomedical Research Centre and GOSH Children’s Charity.
Links
Research in Nature Communications Dr Giovanni Giobbe's academic profile Professor Paolo De Coppi's academic profile UCL Great Ormond Street Institute of Child Health UCL Population Health Sciences NIHR GOSH BRCImage
Credit: Liudmila Chernetska on iStockMedia contact
Poppy Danby
E: p.danby [at] ucl.ac.uk
****
Research on children's brain tumours awarded £1.6m
6 July 2023
Experts at UCL, Queen Mary University of London and Great Ormond Street Hospital are aiming to develop revolutionary treatments for children diagnosed with low-grade brain tumours, following major new funding.
The research team have been awarded £1.6 million by The Brain Tumour Charity to advance knowledge of low-grade brain tumours, how they behave in the body, how to better treat them and how to improve quality of life for children affected.
The research will be carried out in collaboration with researchers at the German Cancer Research Centre (DKFZ) and will continue the ground-breaking work of The Everest Centre*, following a second total investment of £5 million by The Brain Tumour Charity.
More than 400 children are diagnosed with a brain tumour each year in the UK. And, of these, approximately half are low-grade tumours.
Kinder and more effective treatments are needed as 20% of children do not survive for more than 20 years following a diagnosis. The current standard of care, which includes chemotherapy, radiotherapy and high-risk surgery, has a significant impact on a child’s quality of life.
Scientists at UCL will focus their research on tumour biology to understand the genetic make-up of low-grade tumours as this will help to improve the precision of diagnosis and work towards more personalised treatments to benefit patients.
They will also compare key features of low-grade paediatric brain tumours with other tumours in children and will explore how brain tumours protect themselves from the immune system and resist treatment.
Professor Tom Jacques (UCL Great Ormond Street Institute of Child Health) said: “Advancing our understanding of the molecular biology of these tumours will improve the ways in which we can clinically manage treatment. A deeper understanding of low-grade tumours will help us identify targets for new potential treatments.
“Our collaborations in the UK and Germany will allow us to harmonise diagnostic practises across Europe which will benefit those newly diagnosed. And the more data we collect about the genetic make-up of low-grade paediatric brain tumours will only further our ability to give children and their families more hope.
“This is a very exciting project and we look forward to working with everyone at the Everest Centre.”
Research will also focus on improving understanding of how tumour growth is controlled in the body and how ‘sleeping’ (also known as senescent) cells influence tumour growth and respond to treatment, which could help improve treatment options in the future.
Novel artificial intelligence (AI) systems will be developed to improve diagnosis of low-grade brain tumours. Using AI could be particularly useful in countries where molecular testing of tumours is costly.
The researchers at UCL will also play an important role in translating laboratory science into direct patient benefit. They will support the establishment of an innovative clinical trial, known as EPILOGUE, to identify new treatment options for patients.
Ulixertinib, a first-class drug recently discovered by scientists at The Everest Centre as a potential new treatment for low-grade brain tumours in children, will be one of the first drugs tested in the EPILOGUE trial.
Professor JP Martinez-Barbera (UCL Great Ormond Street Institute of Child Health) said: “Thanks to funding from The Brain Tumour Charity, our achievements so far lay down a strong foundation for developing new approaches to treatments for children with low-grade brain tumours.
“Our research aims to use knowledge already gained from work at the Everest Centre to further understand the role of senescence in low-grade brain tumours and identify new vulnerabilities of these brain tumour cells in order to explore novel treatment options for children.
“Our collaborations within UCL, and with partners at Queen Mary University of London and in Germany will enhance our research capability and truly improve options for children with a low-grade brain tumour diagnosis.”
A new quality of life questionnaire will also be introduced to help fully understand the effect of treatments on children.
Professor Darren Hargrave (UCL Great Ormond Street Institute of Child Health) said: “Children diagnosed with brain tumours do not have the outcomes that children with other types of cancer have, and better and kinder treatments are a priority.
“The standard treatment for low-grade brain tumours can include multiple rounds of treatment – including surgery, chemotherapy and radiotherapy – for many years of their lives, and that often has profound long-term effects on their health.
“We want our research to improve the lives of children diagnosed with a brain tumour, and the research we are going to carry out with this funding will enable us to do this.
“It is so important to translate the research we do in the labs into better outcomes for children.”
Meanwhile, researchers at Queen Mary University of London (QMUL) will investigate how tumour cell growth is controlled by the MAPK signalling pathway – a molecular cascade that controls the way cells multiply, survive and die, and is the most frequently altered pathway in paediatric low-grade brain tumours.
*The Everest Centre for Research into Paediatric Low-Grade Gliomas was established in the UK and Germany in 2017 with an initial £5 million funding from The Brain Tumour Charity. It brings together pioneering brain tumour scientists from DKFZ in Germany and UCL and QMUL in London.
Patient story
Zachery Eckworth, now 11 and living in Basingstoke, Hampshire, was just 14 months old when he was diagnosed with an optic nerve glioma.
Zac was growing up just like any boy his age, until his parents, Miriam and Colin, noticed his eye was wobbling. Zac’s parents took him to see the GP who referred him straight to the eye clinic as Zac had banged his eye a few weeks before.
The clinic sent Zac to the local A&E where he had an MRI scan and after an overnight stay, Zac was diagnosed with an optic nerve glioma. These tumours are slow growing and grow in or around the optic nerve, which connects the eye to the brain.
Zac was referred to specialists at Great Ormond Street Hospital the week after his diagnosis where he had to have several rounds of chemotherapy. This was especially difficult because Zac was allergic to some of the chemotherapy drugs and in total had 5 different rounds of treatment.
After the first round of chemotherapy, Zac’s tumour remained stable for nine months, but then it kept growing, and more rounds of chemotherapy were necessary.
Miriam, Zac’s mum, said: “This was a very difficult time for the family. It was hard for Zac and it was hard for us to see him unable to be a child. Our daughter had just been born as well, and we knew the difficulties that chemotherapy would bring for Zac.”
There was some light at the end of the tunnel for Zac and his family. Zac’s tumour was biopsied and was found to have the BRAF-V600E mutation which activates the MAPK signalling pathway, leading to cells dividing uncontrollably and tumour growth. Knowing which mutation to target, Zac’s medical team put him on a trial treatment drug known as dabrafenib. Zac responded well to this drug and has been taking it since he was five.
Zac will remain on this treatment until his teenage years, when doctors will try to stop treatment and monitor how the tumour responds. There was a brief period where treatment was stopped, but the tumour began to grow again, so Zac was put back on it. Zac’s tumour responded well to dabrafenib, and shrank considerably.
Miriam said: “Every day we feel blessed to have been given this life-changing treatment option. It has given Zac the chance to live a relatively normal life. We are incredibly grateful to Professor Hargrave and all of his work and we are thankful for the research that means Zac can do so many of the things 11 year old boys do.”
Zac is substantially visually impaired as a result of his brain tumour. He suffered from hydrocephalus, a build-up of fluid on the brain, and also had lots of chemotherapy at a young age. His school is very supportive and day-to-day he learns braille and they provide him with large print. He also enjoys playing goal ball – a visually impaired sport.
Zac lives with the after-effects of his tumour but he doesn’t let it impact his life too much. He is nearly a black belt in karate. This helped him to build his confidence after surgery. He plays the keyboard and loves to be a DJ in his spare time. He also loves playing video games with his friends.
Miriam said: “Zac has a good quality of life, which allows him to recover emotionally from what he experienced in his younger years. He is able to live a relatively normal life which allows him to have his own identity – this treatment has given him that, it has given us more quality time as a family.
“We are so thankful for the research that has allowed this and praise the work of Professor Hargrave."
Links
Professor Darren hargrave's academic profile Professor JP Martinez-Barbera's academic profile Professor Tom Jacques's academic profile UCL Great Ormond Street Institute of Child Health UCL Population Health SciencesImage
Credit: KatarzynaBialasiewicz on iStockMedia contact
Poppy Danby
E: p.danby [at] ucl.ac.uk
*****
Unlocking the mystery of long-lasting cancer treatment
6 July 2023
Scientists, including UCL experts, have found new insights into why some children have a longer remission than others after receiving CAR T-cell therapy for leukaemia.
The collaborative research project, published in Nature Medicine, used clinical expertise and state-of-the-art computational analysis to identify a genetic signature of CAR T-cells that will be the most effective in the long term.
CAR T-cells are genetically engineered T-cells (a type of immune cell), that are designed to target leukaemia. In recent years, they have become an established treatment option for children with a relapsed or incurable rare form of blood cancer called B-cell acute lymphoblastic leukaemia (B ALL).
One of the key factors that determine whether the treatment will lead to a durable remission in leukaemia – allowing children to live cancer free - is how long the CAR T-cells last in the body.
Until now, little has been known about what makes these cells last and, therefore, whether the treatment is likely to work long-term, without the need for further therapy.
A collaborative research team from across UCL Great Ormond Street Institute of Child Health (UCL GOS ICH), Great Ormond Street Hospital (GOSH) and the Wellcome Sanger Institute, worked with families for years after their CAR T-cell treatment (called AUTO1), as part of the CARPALL study, to begin to build a picture of why some CAR T-cells stay in the body long-term.
This work provides the first stepping-stone in understanding why some CAR T-cells persist. The team aims to build on the signature discovered in this project to identify key markers in cell populations and ultimately understand if there is a way to spot, or even create CAR T-cells that will persist long-term before treatment begins.
Co-senior author, Dr Sara Ghorashian (UCL Great Ormond Street Institute of Child Health and GOSH) said: “This data for the first time shows us the characteristics of long-lasting CAR T-cells which are responsible not just for curing children with ALL in our study but also seen in adults treated with a different CAR T-cell product for a different type of leukaemia. As such, this provides us with confidence that the signature may unlock mechanisms of CAR T-cell persistence more generally and allow us to develop better treatments.
“We are indebted to all of the children and families who make research like ours possible – it is only through their dedication that we are able to build our understanding of these new therapies and build better treatments for children across the world.”
Lead author, Dr Nathaniel Anderson (Wellcome Sanger Institute), said: “Through cutting-edge single cell genomics, we have, for the first time, been able to crack the code of persistence in CAR T-cells in children with great clarity.
“We hope that our research will provide the first clue as to why some CAR T-cells last for a long time – which we know is vital for keeping children cancer-free after treatment. Ultimately, this work will help us to continue to improve this already life-changing treatment.”
The team were able to study cells from 10 children who were enrolled in the CARPALL trial for up to five years after their original CAR T-cell treatment. This has provided them with a new understanding as to why some of these CAR T-cells stay around in a patient’s bloodstream, and why others vanish early – which can, in some cases, allow the cancer to return.
Using techniques that analyse individual cells at a genetic level to understand what they do, the scientists were able to identify a unique “signature” in long-lasting CAR T-cells. The signature suggested that long-lasting CAR T-cells in the blood transform into a different state that enables them to continue policing the patient’s body for cancer cells.
Vitally, this signature was seen across cells and patients as well as in adults treated with a different CAR T-cell product for a different type of leukaemia. But it was not identified in other types of immune cells. This suggested that the signature the authors identified may not only be a marker of these long-lasting cells but could actually be what makes them persist in the body and allows for a longer remission in children.
As part of the study, the researchers identified the key genes in CAR T-cells that appeared to enable them to persist in the body for a long time. Importantly these genes will provide a starting point for future studies to identify markers of persistence in CAR T-cell products as they are made and ultimately improve their effectiveness.
Dr Sam Behjati, co-senior author, Group Lead (Wellcome Sanger Institute and Addenbrooke’s Hospital, Cambridge) said: “This study is a fantastic step forward in our understanding of CAR T-cell persistence and illustrates the power of collaborative science and combining pioneering clinical research with cutting-edge genomic science. It is crucial that we continue to develop and build on these new treatments to help more children with leukaemia across the world.”
Patient story
Studies such as this are only possible because of the dedication of the children and families who take part in research. For scientists to investigate the long-term persistence of cells, children had to continue to donate cells to the study for up to five years after their initial treatment.
Austin was diagnosed with B ALL at the age of two, by the age of eight he’d been through three relapses and extensive treatment including two bone marrow transplants. By the time of his fourth relapse, he had exhausted all conventional therapy options. In October 2016, Austin received an infusion of CAR T-cells as part of the CARPALL clinical trial.
Over six years later and Austin, now 14, is still cancer free, with long-lasting CAR T-cells detectable in his blood. He is just one of 10 children who have been donating samples to this study since their infusions. His dad Scott said: “It’s not an exaggeration to say that if it wasn’t for research Austin wouldn’t be alive. The research teams at GOSH gave us so much, we wanted to give something back. Taking part in this study not only gives us that opportunity but we also hope that Austin’s data will help other families like ours in the future.
“We actually love coming back to GOSH to see the team and keep them a part of our lives. I feel so proud that Austin has been a part of this research journey.
“Austin and his Mum, Louise, with GOSH Research Nurses Jan Chu and Danielle Pinner at one of their recent yearly visits to the hospital post CAR T-cell treatment to donate samples to the study.”
This continued commitment to studies is helping researchers to better understand new, cutting-edge therapies and improve them for future families.
Links
Research in Nature Medicine Dr Sara Ghorashian’s academic profile UCL Great Ormond Street Institute of Child Health UCL Population Health Sciences GOSH Wellcome Sanger InstituteImage
Credit: Ivan-balvan on iStock
- Previous news items 2022
November 2022 Call for Applications for Funding
Application deadline Friday 18th November 2022. Please click on the link below to download a word version of the
 2022 Application Form
2022 Application FormThe Olivia Hodson Cancer Fund invites applications for funding of projects starting after January 2023. Project applications up to a maximum of £15,000 will be considered, however we do encourage pump-priming applications for smaller amounts of approximately £1-5,000.
We would also welcome applications from Allied Health Professionals where R& D approval will not be required.

Applications should be emailed to Anne Anton by Friday 18th November 2022. Applications should be fully costed and registered with R&D. Please see the attachment for further information about the fund and the application form.
Your recommended peer reviewers will be contacted shortly after the deadline. It may speed up your application to let them know in advance that we will be getting in touch. The committee are unable to approve applications without a peer review.
The Committee will meet to review applications shortly after the deadline of 22nd April 2022 and we will shortlist applications to be sent for review. All applicants will be notified about the shortlisting. Following the external review of shortlisted applications, the committee will meet to assess the peer reviews on 13th June. Applicants may be required to attend an allocated slot and present (10mins presentation and 5mins for Q&A).
OHCF Committee
*****************
January 2022 Call for Applications for Funding
Application deadline Friday 22nd April 2022. Please click on the link below to download a word version of the
 2022 Application Form
2022 Application FormThe Olivia Hodson Cancer Fund invites applications for funding of projects starting after August 2022. Project applications up to a maximum of £15,000 will be considered, however we do encourage pump-priming applications for smaller amounts of approximately £1,000 - £5,000.

Applications should be emailed to Anne Anton by Friday 22nd April 20212. Applications should be fully costed and registered with R&D. Please see the attachment for further information about the fund and the application form.
Your recommended peer reviewers will be contacted shortly after the deadline. It may speed up your application to let them know in advance that we will be getting in touch. The committee are unable to approve applications without a peer review.
The Committee will meet to review applications shortly after the deadline of 22nd April 2022 and we will shortlist applications to be sent for review. All applicants will be notified about the shortlisting. Following the external review of shortlisted applications, the committee will meet to assess the peer reviews on 13th June. Applicants may be required to attend an allocated slot and present (10mins presentation and 5mins for Q&A).
OHCF Committee
****
DBC welcomes a new Head of Department
4 January 2022
DBC are delighted to announce that Professor Nick Greene has taken over as Department Head after Professor JP Martinez-Barbera stepped down in December 2021.
Professor Martinez-Barbera will continue his role as Prinicple Investigator to his hugely successful Paediatric Brain and Pituitary Tumours Research Group as well as his role of Deputy Director (Institutional Relations).
We would like to take this opportunity to thank Professor Martinez-Barbera for his excellent leadership of the Department over the last 4 years and to congofessor Greene on his appointment.Previous news items 2021
- Previous news items 2021
Lab-grown ‘mini-stomachs’ could shed light on COVID symptoms in children
14 December 2021
A “lab-grown model” of the human stomach that can be used to study how infections impact the gastrointestinal system, has been developed for the first time by a UCL-led team of international scientists.
The team from Great Ormond Street Hospital (GOSH), UCL Great Ormond Street Institute of Child Health (UCL GOS ICH) and the Istituto Zooprofilattico Sperimentale delle Venezie (Legnaro, Italy), have built on recent advances to grow ‘mini-organs’ in a laboratory, known as organoids. These organoids provide researchers with invaluable tools to study how organs function both when they are healthy and when impacted by disease.
In this study, published in Nature Communications, scientists have for the first time described how to grow mini-stomach organoids, across differing stages of development – fetal, child and adult.
To do this, researchers, based at Zayed Centre for Research into Rare Disease in Children, isolated stem cells from patient stomach samples, and grew them under special conditions in the lab to obtain mini-stomachs in a dish that mimic the behaviour of a human stomach.
As the COVID-19 pandemic progressed, several hospitals reported gastrointestinal symptoms alongside the more usual respiratory effects like coughs and breathing difficulties, particularly in children. Following these cases, the research team, led by Dr Giovanni Giuseppe Giobbe, Professor Nicola Elvassore and Professor Paolo De Coppi from UCL GOS ICH, and Dr Francesco Bonfante from Istituto Zooprofilattico Sperimentale delle Venezie, determined that their mini-stomach model could be used to study how a SARS-CoV-2 infection affects the stomach.
The scientists were able to facilitate the infection of the mini-stomachs from the outside by exposing the surface of the cells to the virus. From this they showed that SARS-CoV-2 could replicate within the stomach, more noticeably in organoids that were grown from the child and late fetal cells, compared to adult and early fetal cells.
The research team were also able to look at the impact of the infection on the cells within the organoids, showing that a specific group of cells, called delta cells that make a hormone called somatostatin, had died, which could explain some of the stomach symptoms seen in patients. The team’s laboratory results mirror the pattern of gastrointestinal symptoms seen in patients of different ages.
Professor Paolo De Coppi, (GOSH Consultant Paediatric Surgeon and UCL GOS ICH Nuffield Professor of Paediatric Surgery), senior author said: “This study has highlighted that SARS-CoV-2 infection may begin to infect the gastrointestinal system via the stomach in children and young babies. We hope that this adds another piece to the puzzle as we try to build our understanding of the impact of the virus across the body. As a research team we are proud to have been able contribute to the global fight against coronavirus in this way, pivoting our research as the need arose.”
The team now plan to continue their work utilising these new mini-stomachs, aiming to study how the stomach develops from early in pregnancy through to adulthood. They also hope to look at the effects of other common gastrointestinal infections.
Dr Giovanni G Giobbe (UCL GOS ICH Senior Research Associate) and co-lead author on the study said: “We have been able to develop the first fetal model of the stomach and have demonstrated that the human gastric organoids can be used to accurately study real-world infections. Developing reliable models of organs that scientists and doctors can study in a lab are vital as they allow us to work out how organ tissue is affected during disease and infection. We want to increase our understanding of how infections impact the stomach so that we can further the search for new treatments.”
Links
UCL Great Ormond Street Institute of Child Health Great Ormond Street Hospital Istituto Zooprofilattico Sperimentale delle Venezie Full paper Professor Paolo De Coppi's academic profileResearch theme: Solid Tumours in Children
Summary: To develop effective, kinder treatments for children with solid tumours, we must explore new therapeutic approaches. The NGTC team’s vision is to bring engineered T cell therapies to the routine treatment of these children, within a decade.
Dr Laura Donovan and Dr Karin Straathof (both UCL Great Ormond Institute for Child Health) and are co-investigators on Team The Virtual Child. The team is led by Professor Dr Stefan Pfister (German Cancer Research Centre) and Professor Richard Gilbertson (University of Cambridge)
Research theme: Solid Tumours in Children
Summary: The first ever learning and data-driven computer model of normal and cancerous nervous system development, to support biological and therapeutic discovery.
Professor Juan Pedro Martinez-Barbera (UCL Great Ormond Institute for Child Health), co-investigator, Team T-SMAC: Targeting Senescence Mechanisms to Arrest Cancer. The international team is led by Professor Scott Lowe (Memorial Sloan-Kettering Cancer Center, US), Professor Manuel Serrano (Institute for Research in Biomedicine, Spain) and Professor Jesus Gil (Imperial College London).
Research theme: Senescence
Summary: Improving the mechanistic understanding and detection of senescence to realise its potential in cancer treatment
Applications should be made to the DBC Admin Team. The deadline for applications is 31st January 2022.
****
Paolo de Coppi is elected President of the EUPSA
29 September 2021
We are delighted to announce that Paolo de Coppi has been elected President of the European Pediatric Surgical Association (EUPSA). EUPSA is the largest Paediatric Surgical Organisation worldwide with more than 800 members from over 50 countries. A true honour and well deserved.
****
Laura Donovan wins SITC-Akoya Special Phenotyping Award
29 September 2021
A huge congratulations to Laura Donovan who has won a SITC Fellowships and Technology Award which helps to support the next generation of cancer immunotherapy and tumor immunology experts through dedicated funding of impactful research.The SITC Fellowships and Technology Awards were established through the Forward Fund to support the development of early career investigators in the field to cultivate the next generation of cancer immunotherapy experts.
****
Research Paper Highlight
29 September 2021
Alcohol-abuse drug disulfiram targets pediatric glioma via MLL degradation
This paper addresses the challenging issue of novel therapies for brain tumours and is from a group, led by David Michod and Jaspar de Boer, including also Stefanie Meier, Sandra Cantilena, John Anderson and Darren Hargrave.
Disulfiram is an old drug, used to help manage alcohol abuse, recently shown to be active against cancer cells. The group showed that disulfiram killed paediatric glioma cells, both cell lines and patient derived cells. They also unravelled the likely mechanism by showing that disulfiram induces degradation of an oncoprotein, which they propose as the novel key target of this old drug and opening up a potential new treatment for paediatric gliomas.
Link to paper in Cell Death and Disease****
Make September Gold!
1 September 2021

September is Childhood Cancer Awareness Month. Every day in the UK, 12 children and young people will receive the devastating news that they have cancer. Of those 12, two will not survive. Of those lucky enough to survive, many will have long-term side-effects that may significantly impact their lives forever.
Show your support this September by wearing a gold ribbon. Limited edition gold ribbon pin badges can be purchased from Children with Cancer UK, please click here for more details.
****
UCL scientists to receive seed funding for most pressing cancer challenges
21 June 2021
Nine UCL scientists have been shortlisted to work on some of the world’s toughest cancer problems, as part of the £80 million Cancer Grand Challenges including three from DBC.

In October 2020, Cancer Grand Challenges, founded by Cancer Research UK and the US National Cancer Institute, dared the global research community to take on nine of cancer’s most pressing issues.
The eight research themes taken forward were: Cachexia (a disorder that causes extreme weight loss and muscle wasting, and can include loss of body fat), e-cigarettes, extrachromosomal DNA, inflammation, macromolecules, normal phenotypes, senescence (the condition or process of deterioration with age), solid tumours in children.
Almost 170 teams across 61 countries submitted bold, innovative ideas, and Cancer Grand Challenges has now announced the 11 teams selected to compete for a share of £80m.
Each team will now receive seed funding to get their ideas off the ground and make their full proposal. Winners will receive £20m and the freedom to unite above boundaries to unleash their scientific creativity.
UCL scientists feature in six of the 11 teams shortlisted.
Dr Martin Pule (UCL Cancer Institute), is co-lead for Team NGTC: Next Generation T cell therapies for childhood cancers. The UCL Translational Research Office (TRO) supported application involves an international team of researchers co-led by Dr Catherine Bollard, (George Washington University Children’s National Hospital) and including from UCL, Professor Sergio Quezada (UCL Cancer Institute), Professor Karen Page (UCL Mathematics), Professor Marc-Olivier Coppens (UCL Chemical Engineering) and Dr Karin Straathof (UCL Great Ormond Institute for Child Health).
****
2020/21 Applications for the Alex Simpson Smith Travelling Fellowship now being accepted
November 2021
The Trustees of the Alex Simpson Smith Trust Fund and Travelling Fellowship Committee wish to encourage use of the fund to support travel and visits to other centres in order to promote academic surgical training and research. Priority will be given to staff and students at the UCL GOS Institute of Child Health and Great Ormond Street Hospital, but applications from other academic or surgical centres in the UK will also be considered. It is envisaged that the Fellowship may be held by staff already working in academic surgery or a closely relevant area, or by students undertaking training in this area, for example as part of the GOSH CC ICH Surgeon Scientist PhD programme Possible purposes of travel under the Fellowship scheme might include periods of training in advanced surgical techniques or technology and surgical research collaborations. Although it is not intended that the awards are solely to attend conferences, where a study visit to a centre can be reasonably combined with attendance at a conference, the cost of the conference will be considered. In order to ensure best use of the limited funds available, all proposals for Travelling Fellowships will be evaluated by an academic sub group of the Alex Simpson Smith Trust Fund and Travelling Fellowship Committee, according to the following administrative process.
Applicants wishing to apply should submit:
A brief outline of their proposed visit, stating the centre they wish to visit and explaining how this will enhance their training and/or research A provisional letter of acceptance from their proposed visit An estimate of their proposed travelling costs and expenses A copy of their CV Approval of their supervising Consultants for this visit should also be shownImage
A microscopic image of the mini stomachs used in the research Credit: Giovanni Giobbe
UCL & GOSH researchers receive funding to improve outcomes for children and young people with cancer
18 March 2021
Researchers at University College London and Great Ormond Street Hospital receive ~£1,7m funding in new Cancer Research UK-Children with Cancer UK Innovation Awards.
The Award is a new initiative to support novel and innovative approaches to childhood cancer research. Co-funded by Cancer Research UK and Children with Cancer UK, five teams of scientists who are leaders in their field have been awarded up to £1 million each to delve into the biology of children’s and young people’s cancers, with the hope of finding new ways to prevent and treat these complex cancers.
Improving outcomes for children and young people whose ALL relapses after treatment
One of the studies awarded this £1m grant is the REVEALL Study (RElapse-specific therapeutic Vulnerability Evaluation in childhood & young adult ALL). This is a joint proposal led by researchers and clinicians from University College London (Cancer Institute and Great Ormond Street Institute of Child Health) and Great Ormond Street Hospital in collaboration with experts from other centres including the Francis Crick Institute and Memorial Sloan Kettering Cancer Center, New York.
Although most children with leukaemia can be cured with standard therapy, treatment can be much more difficult if the disease returns (“relapses”). To address this issue, a nationwide study will be established, recruiting all children in the UK with relapsed leukaemia.
Dr David O’Connor said:
“through the analysis of patient samples we will characterise the leukaemia in unprecedented detail, uncovering the cancer’s genetics and sensitivities to different treatments. This form of personalised medicine will guide which treatments the patients receive, giving them the best chance of survival. We believe our approach will provide direct benefit to children with otherwise untreatable leukaemia. In addition, the wealth of data will provide a key resource for other researchers working on leukaemia, deciphering key mechanisms driving resistance, identifying predictive indicators, commonly called biomarkers, for treatment selection and uncovering new targets for drug development.”
Identifying new targets to treat rhabdomyosarcoma (RMS), a skeletal muscle cancer, by investigating its foetal origins
A second study looks at the biology of RMS, which is largely unexplored, but is thought to originate from cells in the foetus that develop incorrectly. Some of these cells persist in children with RMS when usually they wouldn’t. Dr Sam Behjati at the Wellcome Sanger Institute, and Dr Karin Straathof at UCL GOS ICH/GOSH, want to understand why this happens by building a cell ‘atlas’ – a complete guide to the cells that form RMS. They hope that understanding how RMS develops will help bring to light new targets for treatment.
Dr Karin Straathof said:
“While families of children diagnosed with cancer often ask this question, we do not yet know how cancers like rhabdomyosarcoma develop. By building a detailed map of this cancer and comparing this with what happens during normal development we will get a better understanding of the root of rhabdomyosarcoma. And importantly these insights will provide us with clues of how to develop new treatments.”
Dr Sam Behjati Said:
“Although treatments have dramatically improved over the past few decades, children continue to suffer from rhabdomyosarcoma, with few novel treatment approaches in sight. Moreover, survivors often experience lifelong adverse effects from treatment. I hope that our research will ultimately translate into benefits for children with rhabdomyosarcoma, in particular, better treatments.”
Images
CRUK -CwCUK logo's Prof Marc Mansour, Dr Jack Bartram, Prof Owen Williams, Dr David O'Connor (left to right) Dr Karin Straathof****
Olivia Hodson Cancer Fund

January 2021 Call for Applications for Funding
Application deadline Friday 9th April 2021. Please click the link below for a word version of the 2021 application form.
The Olivia Hodson Cancer Fund invites applications for funding of projects starting after July 2021. Project applications up to a maximum of £20,000 will be considered, however we do encourage pump-priming applications for smaller amounts of approximately £1,000 - £5,000.
Applications should be emailed to Anne Anton Friday 9th April 2021. Applications should be fully costed and registered with R&D. Please see the attachment for further information about the fund and the application form.
Your recommended peer reviewers will be contacted shortly after the deadline. It may speed up your application to let them know in advance that we will be getting in touch. The committee are unable to approve applications without a peer review.
The Committee will meet to review applications shortly after the deadline of 9th April 2021 and we will shortlist applications to be sent for review. All applicants will be notified about the shortlisting. Following the external review of shortlisted applications, the committee will meet to assess the peer reviews in mid June – date to be confirmed. Applicants may be required to attend an allocated slot and present (10mins presentation and 5mins for Q&A).
OHCF Committee
Links
Dr David O’Connor’s research profile Professor Owen Williams’ research profile Professor Marc Mansour’s research profile Dr Jack Bartram, GOSH Consultant Dr Karin Straathof’s research profile Developmental Biology & Cancer Research & Teaching Department, UCL Great Ormond Street Institute of Child Health UCL Cancer Institute Great Ormond Street Hospital NHS Trust CRUK Innovation Awards- Previous news items 2020
Lab-grown mini-organs could offer treatment hope for children with intestinal failure

7 September 2020
Pioneering scientists at Great Ormond Street Hospital (GOSH), the UCL Great Ormond Street Institute of Child Health (ICH) and the Francis Crick Institute have grown human intestinal grafts using stem cells from patient tissue that could one day lead to personalised transplants for children with intestinal failure, according to a study published in Nature Magazine
Many colleagues from the Developmental Biology and Cancer Research and Teaching Deaprtment have been involved in this highly promising study, and full details may be found at this link
Dr Erwin Pauws appointed to be a new UCL MSc Programme Director
Dr Erwin
Pauws of the developmental BIOLOGY of birth defects section (craniofacial malformation research group) to co-lead a UCL MSc Programme
Making the announcement on 18th June 2020 regarding Dr Pauws new role, Prof. Ros Smyth, Director and Professor of Child Health, Great Ormond Street UCL Institute of Child Health stated:
I am delighted to announce the appointment of two new Programme Directors for the MSc in Paediatrics and Child Health and the MSc in Personalised Medicine and Novel Therapies. Dr Erwin Pauws and Dr Haiyan Zhou respectively will be taking on these important roles as co-leads alongside the existing Directors, Professor Helen Bedford and Dr Mark Kristiansen. These are important leadership roles which will be crucial to our success in education over the upcoming years and in particular with our new online intake commencing in the new academic year. Congratulations to both Haiyan and Erwin who have both shown great enthusiasm for the opportunities offered by the positions and who I believe will make many positive contributions to GOS ICH in these roles.
The Developmental Biology and Cancer Research and Teaching Department congratulates Dr Pauws on his well deserved appointment.
Professor Paolo De Coppi elected to the prestigious Academy of Medical Sciences Fellowship

The Academy of Medical Sciences announced on 13th May 2020 they had elected 50 of the UK’s most prominent biomedical and health scientists to their Fellowship, including the internationally renowned Professor Paolo De Coppi, Head of the Stem Cells & Regenerative Medicine Section at UCL Institute of Child Health, Developmental Biology and Cancer.
Developmental Biology and Cancer Research and Teaching Department warmly congratulates Prof. De Coppi on this most laudable achievement.
Further details may be found at the Academy's press release, at the following web address https://acmedsci.ac.uk/more/news/50-leading-biomedical-and-health-scientists-elected-to-the-prestigious-academy-fellowship
GOSH Charity and Sparks award over £1 million for child health research at the Institute
GOSH Charity and Sparks, the children’s medical research charity, have announced funding for five projects at the UCL Great Ormond Street Institute of Child Health (ICH), as part of the UK’s largest funding scheme dedicated to child health research.

Projects include pioneering research to save the hearing of children who are born without sight, supporting the UK arm of a global clinical trial to test whether the breast cancer drug tamoxifen could help children with a rare muscle disorder, and creating an implantable device that supports liver function and could hold the key to reducing toxic chemical levels in the blood and avoiding the need for liver transplant.
This year, the charities’ annual funding scheme will invest £2.3 million in 11 pioneering child health projects around the UK. After an open call for applications in 2019, each proposal was rigorously assessed by expert committees and researchers around the globe. Those selected, including the five projects at the ICH, were rated extremely highly and recognised as having the potential to significantly impact child health.
Projects funded at the ICH:
Professor Nicholas Greene will test a new compound derived from cinnamon that could help lower toxic levels of ammonia and glycine in children with the rare metabolic diseases non-ketotic hyperglycinemia and Urea Cycle Disorders. Dr Giovanni Baranello’s project will support the UK arm of a global trial understanding if the breast cancer drug tamoxifen could help children with the muscle disorder X-linked myotubular myopathy. Professor Jane Sowden (pictured above) will investigate whether replacing the faulty gene that causes deafness in Norrie Disease could save the hearing of boys with the condition, who are born blind. This is a continuation of the pioneering work done by Professor Maria Bitner-Glindzicz, who sadly passed away in 2018. Professor Paul Gissen aims to tackle all symptoms of a complex multi-organ disorder, Arthrogryposis Renal Dysfunction and Cholestasis Syndrome (ARC), with two types of gene therapy at once. The condition affects the liver, kidneys and bone marrow cells. Most patients die in early childhood so new treatments are desperately needed. Dr Hassan Rashidi hopes to develop an implantable and removable ‘liver patch’ to provide liver support to patients with the metabolic condition non-ketotic hyperglycinemia, helping them reduce the toxic levels of glycine without the need for liver transplant.Research Highlights
Paper of the month
The paper of the month this month goes to a group from Developmental Biology and Cancer. Both joint first authors were undergraduates when they completed the work reported in this paper in Dr Gabriel Galea's lab. Nina Short, who was awarded a Child Health Research Summer Internship, and Max Butler was awarded a Wellcome Biomedical Vacation Studentship. The last author in the paper is Gabriel Galea and the other authors are also from this Institute.
The study focusses on the role of the enzyme Rho-associated protein kinase (ROCK) enclosing the posterior neuropore (PNP) in the neural tube. The main finding from the study is that ROCK dependent apical constriction compensates for the PNP widening effects of the inter-kinetic nuclear migration to enable progression of closure of the neural tube.There is also a first person interview with Max and Nina published in the same edition of the journal. A very well done to students and the rest of the research team!
Link to the paper in the Company of Biologists
Links
Research at the UCL Great Ormond Street Institute of Child Health
Professor Nick Greene's academic profile
Dr Giovanni Baranello's academic profile
Professor Jane Sowden' s academic profile
Professor Paul Gissen's academic profile
Dr Hassan Rashidi's academic profile
***
UCL-PKU Strategic Partner Funds: Prof. Nick Greene
UCL professors Nick Greene and Andrew Copp have teamed up with colleagues at Peking University (PKU) to help prevent one of world’s most common birth defects.
*Update 9/3/2020: Professor Nick Greene received around £300,000 from the Joint Global Health Trials scheme, which is funded by the Department for International Development, the Medical Research Council, the National Institute for Health Research and Wellcome Trust. Prof Greene is the principal investigator with co-applicants from UCL GOS Institute of Child Health, UCL Comprehensive Clinical Trials Unit and Peking University. The team also obtained funding from Bo Hjelt Foundation, which will go towards supporting a two-year development trial in Shanxi Province, China as a precursor to a larger study. The development trial is intended to start on 1 April 2020.
UCL has teamed up with Peking University (PKU) in a bid to prevent tens of thousands of babies suffering from spina bifida, one of the world’s most common birth defects.
Researchers at UCL’s Great Ormond Street Institute of Child Health and Comprehensive Clinical Trials Unit are proposing a £5m study of up to 9,000 women in China to confirm initial findings that a vitamin common in fruit, vegetables, meat and nuts could prevent neural tube defects (NTDs) such as spina bifida.
“If successful, it’s a global treatment that could be rolled out and prevent thousands of pregnancies being affected by spina bifida,” said Professor Nick Greene, who is leading the UCL team.
Worldwide, it is estimated that around one in every 1,000 pregnancies are affected by NTDs, with more than 260,000 babies born every year with spina bifida, a severely disabling malformation of the spinal cord.
Women are advised to take supplemental folic acid before and during early pregnancy to reduce the risk of an affected pregnancy. A number of countries, including the USA, Canada and Australia, have also introduced mandatory fortification of food with folic acid and seen a reduction in NTD prevalence.
Nevertheless, some babies still develop spina bifida despite folic acid supplementation or fortification. For example, there are still between 700 and 900 pregnancies affected by neural tube defects each year in the UK.
Research by the UCL team focussed on identifying possible ways to prevent ‘folic acid resistant’ spina bifida. Leading on from their laboratory-based studies on inositol (vitamin B8), they carried out a pilot clinical trial in the UK, among women who had previously experienced one or more affected pregnancies and were therefore at high risk of recurrence. In their next pregnancy, women were randomly given either folic acid and a placebo or folic acid and inositol.
None of the babies born to women who took inositol had spina bifida, but it did occur in some pregnancies where only folic acid was taken. Published in 2016, the findings of this first randomised trial of inositol for prevention of spina bifida indicated the need for a large-scale ‘fully powered’ clinical trial.None of the babies born to women who took inositol had spina bifida, but it did occur in some pregnancies where only folic acid was taken. Published in 2016, the findings of this first randomised trial of inositol for prevention of spina bifida indicated the need for a large-scale ‘fully powered’ clinical trial.
Now Professor Greene and his colleagues hope, with their collaborators at PKU, to use China’s unparalleled database of information on birth defect occurrence to mount a large-scale study to establish whether inositol will work as an effective global treatment to prevent spina bifida, alongside folic acid.
The prevalence of spina bifida in Northern China, where the study will be carried out, is among the highest in the world.
Because of China’s systematic collection of data, the team will be able to find the necessary 9,000 women who have previously suffered a spina bifida pregnancy and are planning another pregnancy so that they can be given inositol.
“Together with its large population, China has a very comprehensive coverage of pregnancy outcomes, which means it is one of the few places that this trial would be possible,” said Professor Greene.
A bid to fund the clinical trial is currently being considered.*
***
 Close
Close