Tissue engineering of corneal tissue equivalents for treatment of ocular surface disorders
Background
Corneal disorders affects over 10 million people worldwide and current treatment strategies often involve replacement of the defective layer with healthy tissue from cadaveric donors. Due to a worldwide donor cornea shortage and the absence of suitable biological scaffolds, recent research has focused on the development of tissue engineering techniques to create alternative therapies.
Aims
- To investigate the potential use of corneal stromal stem cells in the development of engineered corneal tissue equivalents.
- To evaluate the safety and efficacy of Real Architecture for 3D Tissues (RAFT) in the cornea.
- To use tissue engineering approaches to develop methods for delivery of CSSC to patients.
Main publications
Massie I, Levis HJ, Daniels JT (2014) Response of human limbal epithelial cells to wounding on 3D RAFT tissue equivalents: Effect of airlifting and human limbal fibroblasts. Exp Eye Res 127: 196-205
Kureshi AK, Drake RA, Daniels JT (2014) Challenges in the development of a reference standard and potency assay for the clinical production of RAFT tissue equivalents for the cornea. Regen Med 9(2):167-77.
Levis HJ, Peh GS, Toh KP, Poh R, Shortt AJ, Drake RA, Mehta JS, Daniels JT (2012) Plastic compressed collagen as a novel carrier for expanded human corneal endothelial cells for transplantation. PLoS One. 7(11):e50993.
Levis HJ, Menzel-Severing J, Drake RA, Daniels JT. (2012) Plastic compressed collagen constructs for ocular cell culture and transplantation: A new and improved method of confined fluid loss. Curr Eye Res 38(1):41-52.
Investigating cell interactions in the limbal niche
Aims
- Identify soluble factors that regulate stem cell fate using an ex vivo porcine cornea wounding model
- Determine the role of limbal melanocytes in the maintenance of the limbal epithelial progenitors in their native microenvironment
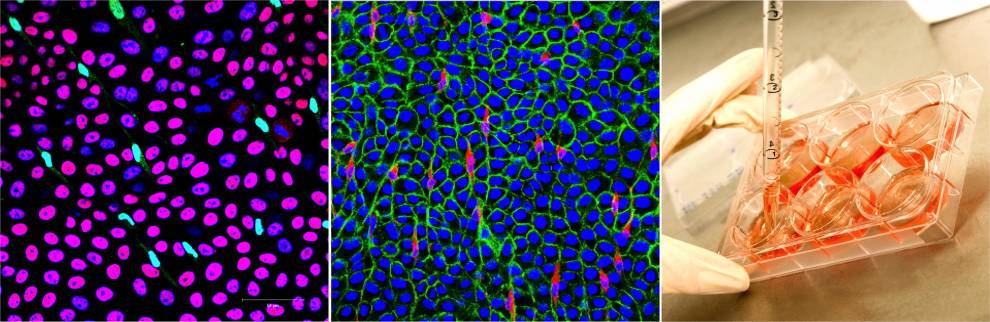
- Tissue engineering of functional corneal tissue equivalents incorporating essential niche elements to support long term limbal epithelial culture and corneal homeostasis.
Main publications
Dziasko MA, Daniels JT. (2016) Anatomical Features and Cell-Cell Interactions in the Human Limbal Epithelial Stem Cell Niche. Ocular Surface 14(3):322-30.
Dziasko MA, Armer HE, Levis HJ, Shortt AJ, Tuft S, Daniels JT. (2014) Localisation of epithelial cells capable of holoclone formation in vitro and direct interaction with stromal cells in the native human limbal crypt. PLoS One 9(4):e94283.
Levis HJ, Massie I, Dziasko MA, Kaasi A, Daniels JT. (2013) Rapid tissue engineering of biomimetic human corneal limbal crypts with 3D niche architecture. Biomaterials 34 (35):8860-8.
Shortt,A.J., Secker,G.A., Munro,P.M., Khaw,P.T., Tuft,S.J., Daniels,J.T. (2007).
Characterization of the limbal epithelial stem cell niche: novel imaging techniques permit in vivo observation and targeted biopsy of limbal epithelial stem cells. Stem Cells 25(6), 1402-1409.
Harris,A.R., Daniels,J.T., Mason,C. (2008). Effect of sub-atmospheric oxygen on the culture of rabbit limbal epithelial stem cells. International Society for Stem Cell Research, Philadelphia
Dziasko MA, Tuft S., Daniels J.T (2015). Limbal melanocytes support limbal epithelial stem cells in 2D and 3D microenvironments. Exp Eye Res. 138:70-9.
 Close
Close