Study shows promising results for predicting side effects in stem cell transplant patients
22 December 2015
Pilot study shows it might be possible to prevent blood cancer patients experiencing severe side effects from donor stem cell transplantation by developing a new way to assess donors’ compatibility.
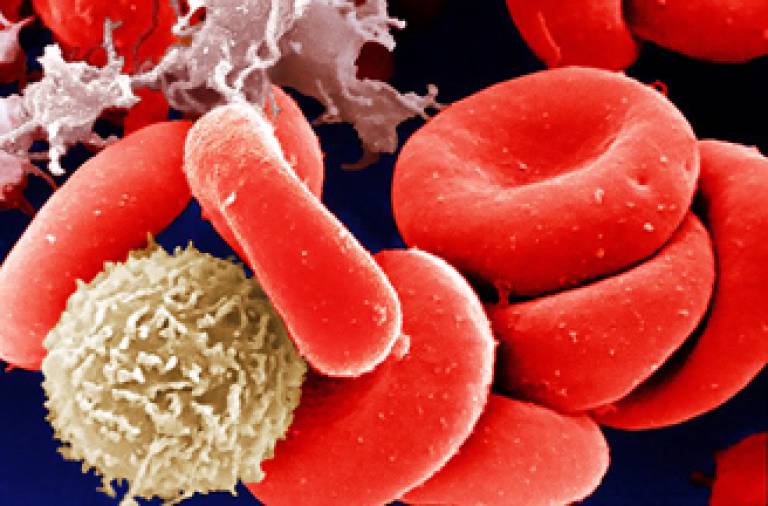
Allogeneic hematopoietic stem cell transplantation (HSCT) is used to treat a variety of blood-related disorders. HSCT is currently one of the only curative treatments available for blood cancers such leukaemia, lymphoma and myeloma. It involves replacing the bone marrow stem cells of a patient following high-dose therapy, with stem cells from a donor.
Even though HSCT can be a very effective treatment, the therapy is not without risk. When such transplants are performed, patients can develop a side effect known as acute graft-versus-host disease (aGVHD) - essentially a donor’s immune system starts to reject the patient. aGVHD can affect the skin, liver and/or gastrointestinal tract. Sometimes complications can be so severe as to cause death. Therefore, the ability to predict which patients are at the highest risk of developing severe aGVHD before a transplantation procedure could improve outcomes significantly, but the question is how?
A team led by researchers from UCL, UCLH, and the Royal Free Hospital, think they may have part of the answer in a new study published in Genome Medicine.
“We thought it would be preferential to develop a biomarker to apply to healthy donors before transplant takes place to assess the likelihood of aGVHD occurring” explains Dr Dirk Paul, who led the study whilst a Research Associate at the UCL Cancer Institute.
“Currently, there is a range of biomarkers (biological markers) that can determine whether aGVHD is likely to develop, so clinicians can apply these to stem cell transplant recipients. However, this type of assessment often happens after a transplant has taken place, so any side-effects a patient experiences can only be managed as it is too late to take any preventative action.”
So, the research team set out to develop an epigenetic tool to stratify donors in order to predict recipients’ responses - ie which donor factors could predict the development of aGVHD before a transplant procedure.
Dr Paul continues: “It is important to note that we used distinctive donor pairs for this pilot study - all donor pairs were siblings, which reduced the confounding issues that would arise using unrelated pairs. This allowed us to gather clear epigenetic readouts that would give us the basis for accurate prediction”.
The team discovered a series of biomarkers prevalent in donors that were associated with an increased chance of developing a severe aGHVD response in recipients.
“We are optimistic - the promising results of our research have enabled us to secure further funding to validate our findings and expand to further donor groups, including unrelated donors where the burden of aGHVD is more prevalent and an accurate biomarker could significantly improve patient outcome.” says Dr Paul.
The research framework that will host the follow-up work of the study is the National Institute for Health Research (NIHR) Blood and Transplant Research Unit (BTRU) in Stem Cells and Immunotherapy at UCL in partnership with NHS Blood and Transplant (NHSBT).
BTRU Scientific Director, Professor Karl Peggs, commented: “The mission of the BTRU is to translate novel academic research findings into the clinical arena in order to provide meaningful benefits to a broad range of patients. This research has the potential to contribute to this key goal and we are excited to see the results of the next phase of validation, and to understand more regarding the biological mechanisms underlying these findings”.
The study was funded by the EU-FP7 Project BLUEPRINT, Barts Charity, Anthony Nolan and Wellcome Trust.
Further information
Research paper: www.genomemedicine.com/content/7/1/128 'A donor-specific epigenetic classifier for acute graft-versus-host disease severity in hematopoietic stem cell transplantation'
 Close
Close

