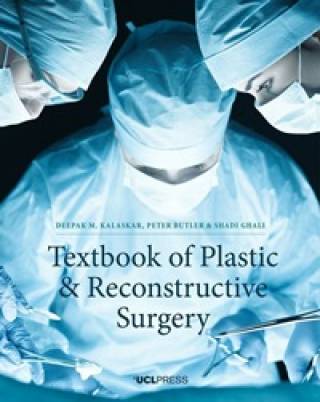
Graduate Taught Study
Our innovative postgraduate programmes are taught by academics and clinicians at the forefront of scientific developments and patient care. Many of our specialist programmes give you the opportunity to discuss ideas with globally leading experts and share your knowledge and experiences with peers from multidisciplinary backgrounds. We offer full-time, part-time, and distance-learning options so you can study in a way that works for you.
Applications are open
We are currently accepting applications for 2024 entry. Find your ideal course and apply today.
About our courses
What our students say
"I would definitely recommend this course to others if they are interested and passionate about supporting patients in pain but also want to learn on a flexible basis. The opportunity of studying with a mix of healthcare professionals with varied working background brings different experiences and opportunities to learn something new from others, which is great. Following this course, I hope it will fuel my career trajectory working in Chronic Pain Management in the community."
See Harriet's story
Funding your studies
UCL offers a range of financial awards aimed at assisting both prospective and current students with their studies. Discover more information about potential funding opportunities:

 Close
Close