Starting HIV treatment early improves patient outcomes
27 May 2015
A major international randomised clinical trial has found that HIV-infected individuals have a considerably lower risk of developing AIDS or other serious illnesses if they start taking antiretroviral drugs sooner, when their CD4+ T-cell count-a key measure of immune system health-is higher, instead of waiting until the CD4+ cell count drops to lower levels.
The trial was conducted as a collaboration between the University of Minnesota, the Medical Research Council Clinical Trials Unit (MRC CTU) at UCL, the University of Copenhagen, the University of New South Wales in Sydney and the Veterans Affairs Medical Center in Washington, D.C
Together with data from previous studies showing that antiretroviral treatment reduced the risk of HIV transmission to uninfected sexual partners, these findings support offering treatment to everyone with HIV.
The new finding is from the Strategic Timing of AntiRetroviral Treatment (START) study,
the first large-scale randomized clinical trial to establish that
earlier antiretroviral treatment benefits all HIV-infected individuals.
The National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, provided primary funding for the START trial. Though the study was expected to conclude at the end of 2016, an interim review of the study data by an independent data and safety monitoring board (DSMB) recommended that results be released early.
"We now have clear-cut proof that it is of significantly greater health benefit to an HIV-infected person to start antiretroviral therapy sooner rather than later," said NIAID Director Dr Anthony S. Fauci. "Moreover, early therapy conveys a double benefit, not only improving the health of individuals but at the same time, by lowering their viral load, reducing the risk they will transmit HIV to others. These findings have global implications for the treatment of HIV."
This provides a very strong rationale for offering treatment to all HIV positive individuals as soon as they are diagnosed
Professor Ab Babiker
"This is an important milestone in HIV research," said Dr Jens
Lundgren of the University of Copenhagen and one of the co-chairs
of the START study. "We now have strong evidence that early treatment
is beneficial to the HIV-positive person. These results support treating
everyone irrespective of CD4+ T-cell count."
The START study, which opened widely in March 2011, was conducted by the International Network for Strategic Initiatives in Global HIV Trials (INSIGHT) at 215 sites in 35 countries. The trial enrolled 4,685 HIV-infected men and women ages 18 and older, with a median age of 36. Participants had never taken antiretroviral therapy and were enrolled with CD4+ cell counts in the normal range-above 500 cells per cubic millimeter (cells/mm3).
Approximately half of the study participants were randomized to initiate antiretroviral treatment immediately (early treatment), and the other half were randomized to defer treatment until their CD4+ cell count declined to 350 cells/mm3. On average, participants in the study were followed for three years.
"We know from previous trials that ART reduces the risk of transmission of HIV," said Professor Ab Babiker (MRC CTU at UCL), one of the co-chairs of the START study. "The findings from START clearly demonstrate that early treatment is also of benefit to the individual. This provides a very strong rationale for offering treatment to all HIV positive individuals as soon as they are diagnosed."
The study measured a combination of outcomes that included serious AIDS events (such as AIDS-related cancer), serious non-AIDS events (major cardiovascular, renal and liver disease and cancer), and death. Based on data from March 2015, the DSMB found 41 instances of AIDS, serious non-AIDS events or death among those enrolled in the study's early treatment group compared to 86 events in the deferred treatment group. The DSMB's interim analysis found risk of developing serious illness or death was reduced by 53 percent among those in the early treatment group, compared to those in the deferred group.
Rates of serious AIDS-related events and serious non-AIDS-related events were both lower in the early treatment group than the deferred treatment group. The risk reduction was more pronounced for the AIDS-related events. Findings were consistent across geographic regions, and the benefits of early treatment were similar for participants from low- and middle-income countries and participants from high-income countries.
"Early ART initiation has been advocated by some investigators in the past, but it is the START trial that provides strong evidence to support the strategy based not only on clinical benefit but also on lack of harm for the individual," explained Dr Alejandro Arenas-Pinto (MRC CTU at UCL and UCL Epidemiology & Health Care), trial Chief Investigator for the UK. "The discussion between patients and clinicians on when to start ART would, from now on, be evidence-based."
Prior to the START trial, there was no randomized controlled trial evidence to guide initiating treatment for individuals with higher CD4+ cell counts. Previous evidence to support early treatment among HIV-positive people with CD4+ cell counts above 350 was limited to data from non-randomized trials or observational cohort studies, and on expert opinion.
START is the first large-scale
randomized clinical trial to offer concrete scientific evidence to
support the current U.S. HIV treatment guidelines,
which recommend that all asymptomatic HIV-infected individuals take
antiretrovirals, regardless of CD4+ cell count. Current World Health
Organization HIV treatment guidelines recommend that HIV-infected
individuals begin antiretroviral therapy when CD4+ cell counts fall to
500 cells/mm3 or less.
In light of the DSMB findings, study investigators are informing all participants of the interim results. Participants will be offered treatment if they are not already on antiretroviral therapy, and they will continue to be followed through 2016.
The international research team included Professor Andrew Phillips (UCL Infection & Population Health), one of the key statisticians involved with data analysis, who collaborates with Copenhagen HIV Programme.
The trial was sponsored by the university of Minnesota and run through their Statistics and Data Management Centre (SDMC). The Medical Research Council Clinical Trials Unit (MRC CTU) at UCL in collaboration with the University of Copenhagen, the University of New South Wales in Sydney and the Veterans Affairs Medical Center in Washington, D.C coordinated the trial across the world.
Links
- Announcement by the National Institutes of Health
- Professor Ab Babiker's academic profile on IRIS
- Dr Alejandro Arenas-Pinto's academic profile on IRIS
- Professor Andrew Phillips' academic profile on IRIS
- Medical Research Council Clinical Trials Unit at UCL
- National Institute of Allergy and Infectious Diseases
- National Institutes of Health
Images
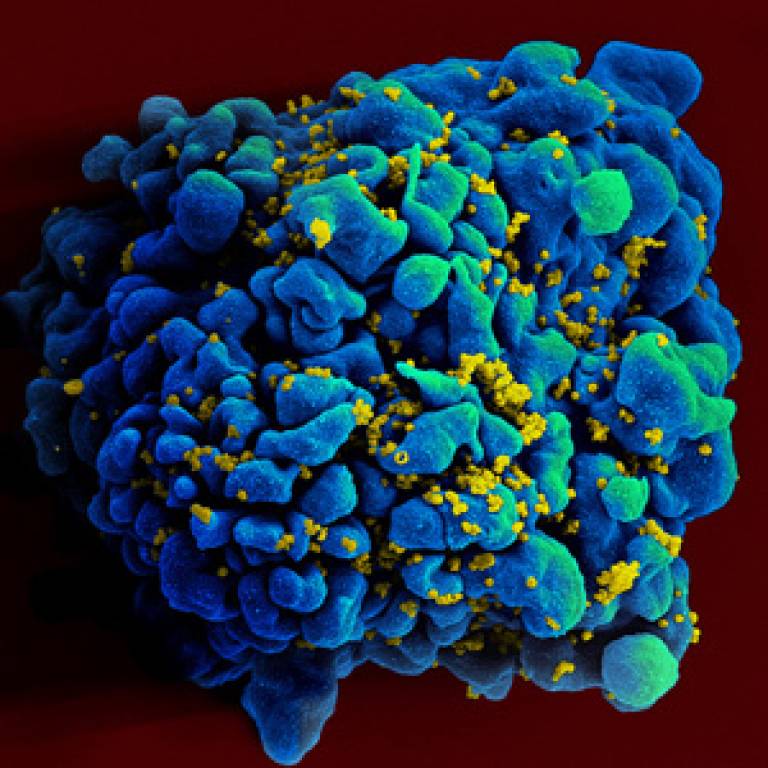
- Scanning electromicrograph of an HIV-infected H9 T cell (courtesy of NIAID on Flickr)
Source
Media contact
Harry Dayantis
Tel: +44 (0)20 3108 3844
Email: h.dayantis [at] ucl.ac.uk
 Close
Close

