Promising pre-clinical results for modified antibody targeting CD25
15 May 2017
Interest in a promising cancer target has been reignited after the publication of pre-clinical research highlighting the potential of using an optimised antibody, targeting CD25, for the treatment of established tumours.
The study, published in medical journal Immunity, emphasises the relevance of CD25 as a target, with findings demonstrating effective eradication of tumours in mice when using a modified anti-CD25 antibody in conjunction with a checkpoint blocking antibody (a therapy that serves to activate the immune response against cancer).
T cells are a key component of our immune system. It is well established that a particular type of T cell known as a regulatory T cell (Treg cell) plays a major role in suppressing the body’s immune response, in health, this is essential for maintaining immune balance.
However, it has been consistently shown that Treg cells can contribute to tumour development and growth in mouse models. Further, in humans, a high number of Treg cells - coupled with low numbers of effector T cells (Teff cells) - is associated with poor outcomes in multiple solid cancers. Concordantly, most studies to date support the idea that targeting Treg cells, either through depletion or modification of activity, can be therapeutically beneficial.
“We’re very interested in regulatory T cells, as we know that they definitely play a role in tumour development,” says Dr Frederick Arce Vargas, Research Associate, UCL Cancer Institute and co-lead author of the study. “In tumours that are highly infiltrated by those cells, they can promote tumour growth by suppressing the body’s immune system - Treg cells act like brakes on the immune response, so we’re investigating ways of eliminating these cells.”
Dr Arce Vargas and his colleagues are not alone in this approach, scientists have been trying to eliminate Treg cells for well over a decade:
“Over the years, many targets on T cells have been identified,” explains Dr Arce Vargas, “One of them is a molecule called CD25, which is a cytokine receptor and is expressed almost exclusively on Treg cells, so it’s an attractive target to focus on - you can use an antibody to identify CD25 and then that antibody can shut down the cells that express it.”
Which sounds fairly straightforward, apart from the fact that previous experiments using this approach have produced discouraging results. Until now.
Right target, wrong antibody
“Pre-clinical studies using anti-CD25 antibodies in mice were very disappointing, they showed that when the anti-CD25 antibody was used before a tumour develops, it was effective but once the tumour was established it didn’t work, this is obviously very impractical for application in humans.” says Dr Arce Vargas.
“In our study, we revisited the CD25 molecule and the antibody that attaches to it, worked out why the antibody wasn’t working - and fixed it. The modified antibody now works, and it works very well!”
The team discovered that the design of the antibody was not optimal, and incapable of eliminating Treg cells within a tumour itself due to high expression of an inhibitory receptor that doesn’t allow the antibody to work. Once this mechanism was understood, the researchers could take steps to change the antibody to solve the problem.
The next step for the team was to combine the new and improved antibody with another antibody known to have anti-tumour activity; a checkpoint blocking antibody called anti-PD-1. The results were remarkable.
“We found that when we combined anti-PD-1 with anti-CD25 - the antibody we had modified - there was a synergistic effect - the two antibodies worked in combination to promote complete tumour eradication,” says Dr Andrew Furness, Medical Oncologist/Cancer Researcher and co-lead author of the study. “In our models, impressive responses against established solid tumours were observed, with no evidence of immune-related toxicity. It’s early days yet, but we are excited about the results.”
From lab to clinic
The translation of the team’s findings to the clinic is a tantalising prospect but there is a great deal of work to do before that could happen. Researchers now need to test combinations using anti-CD25 with other checkpoint inhibitors and a human anti-CD25 antibody for cancer treatment will need to be developed. Going forward, senior study authors, Dr Sergio Quezada, Team Leader of the Cancer Immunology Unit and Professor Karl Peggs, Professor of Transplant Science and Cancer Immunotherapy, will be progressing the research in collaboration with Tusk Therapeutics and Cancer Research Technology (Cancer Research UK’s commercial arm).
Dr Quezada concludes: “The recently published results demonstrate the relevance of CD25 as a therapeutic target and I believe that it shows a clear rationale for progressing it into a therapeutic setting.”
Research support includes Cancer Research UK, NIHR University College London Hospitals Biomedical Research Centre, Bloodwise and the Sam Keen Foundation/NIHR Royal Marsden Hospital Trust Biomedical Research Centre.
Further information
- Paper 'FC-Optimized Anti-CD25 Depletes Tumour-Infiltrating Regulatory T-cells and Synergizes with PD1 Blockade to Eradicate Established Tumours.' Immunity
- Dr Sergio Quezada academic profile
- Professor Karl Peggs academic profile
- Dr Frederick Arce Vargas academic profile
- Dr Andrew Furness academic profile
- Immune Regulation and Tumour Immunotherapy Research Group - Dr Sergio Quezada
- Image: antibody illustration, Shutterstock
Related news
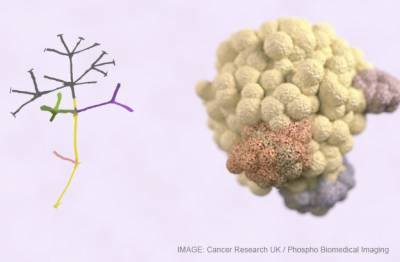
New genetics discovery paves the way to transform immunotherapy treatment
An international team of scientists, led by Dr Sergio Quezada and Professor Charles Swanton, have made a groundbreaking discovery in understanding how the genetic complexity of cancerous tumours can be recognised and exploited by the immune system, even when the disease is at its most advanced stages.
Accelerating Immunotherapy with £5m award
Cancer Research UK has awarded one of the first 2015 Centres Network Accelerator Awards to the CRUK-UCL Centre. The award will fund a network of scientists to track immune responses in cancer patients receiving immunotherapy, and to develop more effective treatments with fewer side-effects.
 Close
Close